-
PDF
- Split View
-
Views
-
Cite
Cite
Hoda Khorasani, Jonas Eiberg, Janne Bigaard, Idiopathic pseudoaneurysm in a patient with breast implants, Journal of Surgical Case Reports, Volume 2016, Issue 7, July 2016, rjw128, https://doi.org/10.1093/jscr/rjw128
Close - Share Icon Share
Abstract
Aneurysms and pseudoaneurysms of the internal mammary artery (IMA) are rare and the etiology uncertain although iatrogenic causes have been described. A 64-year-old woman suffered hematoma and bleeding from a pseudoaneurysm probably originating from a branch of the right IMA 16 years after breast implant surgery. After clinical assessment, the patient underwent surgery with resection of the aneurysm and ligation of the arterial branch. No early postoperative complications were reported. Pseudoaneurysms in small vessels such as the IMA or its branches are not well described in the literature. Proper diagnosis with imaging is of importance in order to determine treatment as each case is unique. Some cases can be managed conservatively.
Introduction
Development of pseudoaneurysms and true aneurysms of the internal mammary artery (IMA) or its branches are rare and to date <15 cases have been described in the literature [1–4]. Pseudoaneurysms are most often iatrogenic or secondary to trauma.
Depending on the cause and intended treatment, computerized tomography (CT), computerized tomography angiography (CTA), magnetic resonance imaging (MRI), magnetic resonance angiography (MRA) or ultrasonography can visualize the aneurysm. Imaging modality is chosen based on several factors such as cause of vascular damage, location and patient morbidity. Ultrasonography is the most used modality. CT and MRI scans are used following severe trauma in order to detect possible related injuries. CTA is a minimally invasive method with catheterization of a vessel and injection of an iodine-rich contrast. MRA is non-invasive and is used in cases where a less invasive imaging method is required. In some cases, MRI or MRA is contraindicated, for example when the patient had foreign material such as metal, clips or a pacemaker inserted.
If not assessed properly with clinical examination and imaging, a possible active bleeding from a pseudoaneurysm can be overseen and subsequently cause significant tissue damage if ruptured.
To our knowledge, this is the third case report describing a pseudoaneurysm in a possible branch of the IMA [5, 6].
Case report
A 64-year-old woman with no comorbidities was referred to the department of vascular surgery experiencing pain and hematoma of her right breast. Sixteen years earlier, she had uncomplicated breast implants for cosmetic reasons. An ultrasound showed a 10 × 10 mm aneurysm located in the upper medial quadrant of her right breast. The aneurysm was located <10 mm under the skin in close relation to the breast implant (Figs 1 and 2).
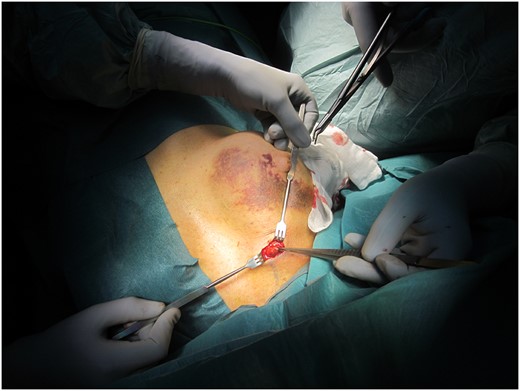
Perioperative image showing the location of the pseudoaneurysm, upper medial quadrant of the right breast and the healing hematoma of the right breast.

All the preoperative blood tests were normal. The aneurysms’ location was marked with ink followed by open resection of the aneurysm including clips ligation of the afferent and efferent artery. The pseudoaneurysm was probably located in a branch of the right IMA. Open ligation was performed as requested by the patient. There was no suspicion of a potential malignant process, and therefore the patient could have been treated conservatively as well. Because of the small vessel size, thrombin injection was ruled out. The patient was discharged uneventful the same evening.
Thirty days postoperatively, the patient was seen in the outpatient clinic for a follow-up with a healed scar and no discomfort. The hematoma of the right breast had regressed, and a new ultrasound of the breasts showed no vessel abnormalities. Histology revealed a partly thrombosed pseudoaneurysm.
Discussion
Treatment options for pseudoaneurysms and true aneurysms of the IMA are the same. The pathophysiology differs depending on the cause. Little is known about pseudoaneurysms in branches of the IMA. Infection around steel wires after sternotomy or trauma in the area could explain its occurrence [4–7, 9]. Although the extent of idiopathic cases is unknown, one should have this in mind when no underlying vascular disease or apparent explanation for a hematoma in the chest occurs.
The main treatment options are either embolization or open ligation. Ultrasound-guided compression, ultrasound-guided thrombin injection or arteriography with coil embolization are the options when an open ligation is not preferred [8]. Potential complications to coil embolization in superficial vessels are not well described in the literature. However, a possible complication could be the formation of an irritating fibrous cap in the area.
In cases of extensive bleeding, open surgery and ligation is naturally preferable if compression does not stop the bleeding. In surgically high-risk patients or when a less invasive method is needed, endovascular coil embolization is often performed. In one case, successful treatment with ultrasound-guided compression was obtained [10]. For some patients, this might be an option instead of more invasive methods.
In this case, color Doppler ultrasonography showed the location of the pseudoaneurysm. Open ligation was performed because the pseudoaneurysm was painful and a palpable tumor was located at 2D (upper medial quadrant of the breast) in the cleavage.
Although not well explained in the literature in association with breast implants, pseudoaneurysms in the IMA or a branch of it, may be a postoperative complication following breast implant surgery. The severity however might not be as pronounced as in other cases and not in need of surgical treatment. Therefore, the actual amount of possible pseudoaneurysms in women with implants is unknown. In the presented case, we believe the pseudoaneurysm had no relation to the previous breast surgery and is therefore an idiopathic de novo event.
As symptoms of pseudoaneurysms in smaller vessels are relatively mild and presented at a late stage, the clinical evaluation of the patient is of importance. Similar to the presented case, many patients present themselves with a pulsatile expanding mass and hematoma in the area.
In general, surgery may not be relevant in asymptomatic patients or when the hematoma has healed. However, clinical assessment and evaluation with ultrasonography is required in order to rule out active bleeding.
Pseudoaneurysms in the IMA or its branches are rare and most often caused by trauma. Idiopathic cases have been reported, but the incidence is unknown.
Conflict of interest statement
None declared.



