-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammed Muneer, Ali Alkhafaji, Ayman El-Menyar, Talal Al-Hetmi, Habib Al-Basti, Hassan Al-Thani, Intravascular extra-digital glomus tumor of the forearm, Journal of Surgical Case Reports, Volume 2016, Issue 7, July 2016, rjw124, https://doi.org/10.1093/jscr/rjw124
Close - Share Icon Share
Abstract
Intravascular glomus tumor in the forearm is very rare and usually presents with persistent pain and focal tenderness. The diagnosis of this condition can be easily missed or delayed. There is no successful treatment so far other than surgical excision in most of cases. We presented a 45-year-old female presented with intravascular glomus tumor in her left forearm. The swelling was excised and the post-operative course was uneventful. Intravascular glomus tumor of the forearm is extremely rare and the persistent pain and tenderness are very suspicious. Diagnostic imaging may not be indicated in every case.
Introduction
A glomus tumor is a benign vascular tumor that originates from the smooth muscle cells of the glomus body that involved in thermal regulation [1, 2]. It accounts for 1–2% of the soft tissue tumors of the hand [3, 4]. Subungual glomus tumors (75–90%) are more common because of the high concentration of glomus bodies [1, 5]. Extra-digital presentations mainly reported in the palm, wrist, forearm, foot, bone, stomach, colon, cervix and mesentery [5]. Intravascular glomus tumors are extremely uncommon especially that originate from the intravascular layer of the forearm [5–9]. Extra-digital glomus tumors are usually presented with pain and localized tenderness [1, 2]. The diagnosis is frequently delayed due to lack of awareness among physicians and low level of suspicion [1, 2]. A comprehensive physical examination, detailed medical history, in-depth imaging and early surgical excision upon clinical suspicion may prevent delayed or incorrect diagnosis [9]. We report a case of intravascular glomus tumor in the forearm of a 45-year-old female managed successfully by surgical incision.
Case presentation
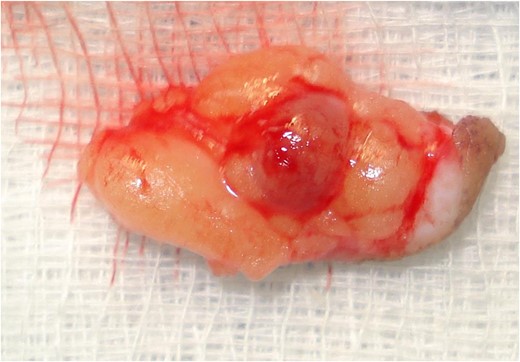
A 45-year-old female presented with a persistently tender and painful swelling in her left forearm for more than 2 years. The lesion was of a small size (1 × 2 cm size) as shown in Fig. 1. However, no sensory alteration or temperature hypersensitivity was observed. The patient denied any family history of similar condition or traumatic injury to the forearm. The swelling was excised (Fig. 2). Interestingly, a superficial vein was feeding the lesion. Therefore, the feeding vein was cauterized and the lesion was sent for histopathology that confirms the diagnosis of intravascular glomus tumor.

Discussion
Beham and Fletcher [6] described the origin of glomus tumor histogenetically as they derive from intramural epithelioid cells of the venous part of an arteriovenous anastomosis. Glomus tumor can be classified as digital/ subungual lesions or extra-digital, solitary or multiple, sporadic or familial lesions. Intravascular glomus tumors are extremely rare [5]. There is marked predilection for fingers particularly subungual followed by palm, wrist, forearm and foot in occurrence of glomus tumors. To the best of our knowledge, only few cases of intravascular glomus tumor in forearm were reported in the medical literature published in English (Table 1) [1, 5–10]. Recently, Temiz et al. [1] described five extra-digital cases (four males and one female) with a mean age of 35 years. All treated surgically (two lesions were located at the arm region, two lesions at the crural region and one lesion at the sternal area).
| Author (year) . | Country . | Age, gender . | Immunohistology . |
|---|---|---|---|
| Beham and Fletcher (1991) [6] | Austria | 40, Male | Positive for vimentin, actin, myosin, S-100 protein and neurofilaments |
| Googe and Griffin (1993) [7] | USA | 66, Male | Positive for vimentin, smooth muscle actin and muscle specific actin; negative for desmin, factor VIII-related antigen, epithelial membrane antigen, cytokeratins, S-100 protein and chromogranin |
| Acebo et al. (1997) [8] | Spain | 79, Female | Positive for vimentin, alpha-smooth-muscle actin and collagen IV |
| Lee et al. (2010) [9] | Canada | 81, Male | Smooth muscle actin immunoreactivity but negative for keratin and S-100 |
| George et al. (2012) [10] | UK | 65, Male | Positive staining with smooth muscle actin, vimentin and CD34. They did not stain with S-100, MNF-116 or CD31. Reticulin and elastic Van Gieson stains highlighted the involvement of the vein wall described. |
| Temiz et al. (2016) [1] | India | Two cases out of 5a | Not mentioned |
| Lee et al. (2014) [5] | South Korea | 44, Female | Smooth muscle actin |
| Present case | Qatar | 45, Female | Positive for actin and S-100 protein |
| Author (year) . | Country . | Age, gender . | Immunohistology . |
|---|---|---|---|
| Beham and Fletcher (1991) [6] | Austria | 40, Male | Positive for vimentin, actin, myosin, S-100 protein and neurofilaments |
| Googe and Griffin (1993) [7] | USA | 66, Male | Positive for vimentin, smooth muscle actin and muscle specific actin; negative for desmin, factor VIII-related antigen, epithelial membrane antigen, cytokeratins, S-100 protein and chromogranin |
| Acebo et al. (1997) [8] | Spain | 79, Female | Positive for vimentin, alpha-smooth-muscle actin and collagen IV |
| Lee et al. (2010) [9] | Canada | 81, Male | Smooth muscle actin immunoreactivity but negative for keratin and S-100 |
| George et al. (2012) [10] | UK | 65, Male | Positive staining with smooth muscle actin, vimentin and CD34. They did not stain with S-100, MNF-116 or CD31. Reticulin and elastic Van Gieson stains highlighted the involvement of the vein wall described. |
| Temiz et al. (2016) [1] | India | Two cases out of 5a | Not mentioned |
| Lee et al. (2014) [5] | South Korea | 44, Female | Smooth muscle actin |
| Present case | Qatar | 45, Female | Positive for actin and S-100 protein |
aDetails of individual cases were not mentioned.
| Author (year) . | Country . | Age, gender . | Immunohistology . |
|---|---|---|---|
| Beham and Fletcher (1991) [6] | Austria | 40, Male | Positive for vimentin, actin, myosin, S-100 protein and neurofilaments |
| Googe and Griffin (1993) [7] | USA | 66, Male | Positive for vimentin, smooth muscle actin and muscle specific actin; negative for desmin, factor VIII-related antigen, epithelial membrane antigen, cytokeratins, S-100 protein and chromogranin |
| Acebo et al. (1997) [8] | Spain | 79, Female | Positive for vimentin, alpha-smooth-muscle actin and collagen IV |
| Lee et al. (2010) [9] | Canada | 81, Male | Smooth muscle actin immunoreactivity but negative for keratin and S-100 |
| George et al. (2012) [10] | UK | 65, Male | Positive staining with smooth muscle actin, vimentin and CD34. They did not stain with S-100, MNF-116 or CD31. Reticulin and elastic Van Gieson stains highlighted the involvement of the vein wall described. |
| Temiz et al. (2016) [1] | India | Two cases out of 5a | Not mentioned |
| Lee et al. (2014) [5] | South Korea | 44, Female | Smooth muscle actin |
| Present case | Qatar | 45, Female | Positive for actin and S-100 protein |
| Author (year) . | Country . | Age, gender . | Immunohistology . |
|---|---|---|---|
| Beham and Fletcher (1991) [6] | Austria | 40, Male | Positive for vimentin, actin, myosin, S-100 protein and neurofilaments |
| Googe and Griffin (1993) [7] | USA | 66, Male | Positive for vimentin, smooth muscle actin and muscle specific actin; negative for desmin, factor VIII-related antigen, epithelial membrane antigen, cytokeratins, S-100 protein and chromogranin |
| Acebo et al. (1997) [8] | Spain | 79, Female | Positive for vimentin, alpha-smooth-muscle actin and collagen IV |
| Lee et al. (2010) [9] | Canada | 81, Male | Smooth muscle actin immunoreactivity but negative for keratin and S-100 |
| George et al. (2012) [10] | UK | 65, Male | Positive staining with smooth muscle actin, vimentin and CD34. They did not stain with S-100, MNF-116 or CD31. Reticulin and elastic Van Gieson stains highlighted the involvement of the vein wall described. |
| Temiz et al. (2016) [1] | India | Two cases out of 5a | Not mentioned |
| Lee et al. (2014) [5] | South Korea | 44, Female | Smooth muscle actin |
| Present case | Qatar | 45, Female | Positive for actin and S-100 protein |
aDetails of individual cases were not mentioned.
The subungual lesions reported to be more common in women than in men, which are approximately three times [1–3]. However, the review of previous case reports on extra-digital glomus tumors in the forearm revealed no gender predilection [5–9]. All reported cases were among adults with age ranging from 40 to 81 years [5–9].
These reports also revealed the presentation as persisting pain and focal tenderness, subcutaneous nodules or a mass with a variable symptoms [5–9]. Lee et al. [9] reported a 7-year history of chronic pain and focal tenderness of the forearm in a 44-year-old woman. Acebo et al. [8] also reported a case of glomus tumor in the forearm in which a 79-year-old woman presented with a history of pain and the dimension of the tumor was 14 cm, which is the largest intravenous growth ever reported. Our case also presented with a swelling in the forearm with a history of pain for more than 2 years with severe tenderness.
In addition, there was no sensory alteration or temperature hypersensitivity observed. This was in line with previously reported cases since none of them reported sensory alterations or temperature hypersensitivity that is more common with the subungual lesions [5–9]. Therefore, the clinical presentation of intravascular glomus tumors is variable. When a patient with a glomus tumor presents with a clear history of painful, focally tender and ‘palpable’ subcutaneous nodule or swelling; then the need for magnetic resonance imaging study is unjustified clinically and practically, unless it is requested for academic purpose. Ultrasound imaging could be useful in some cases. Therefore, most of the reported cases including ours where studied only histologically. Previous histological reports revealed that the neoplastic cells were positive for vimentin, smooth muscle actin and muscle specific actin [6–8].
There is no treatment for a glomus tumor except surgical excision; however, if the lesion is not palpable, it can be easily missed or confusing with other diagnoses such as neuralgia, arthritis and psychosomatic pain [5]. Small lesions can be treated with laser ablation using argon or carbondioxide lasers, sclerotherapy using sodium tetradesyl or hypertonic saline solution [1]. Recurrence is infrequent and is usually due to incomplete excision and fortunately; the conversion to a malignant tumor is reported to be very rare; about <1% [2, 5].
Conclusions
Intravascular glomus tumor of the forearm is extremely rare and the persistent symptoms of pain and tenderness are very suspicious. In such clinical presentation, diagnostic imaging may not be indicated in every lesion.
Competing interests
The authors declare that they have no competing interests and no financial issue to disclose.
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
Ethics approval
A waiver of consent was granted as the patient data were retrieved anonymously with confidentiality and the case report was approved by the medical research center at Hamad Medical Corporation with IRB #16141/16.



