-
PDF
- Split View
-
Views
-
Cite
Cite
Masahiro Shiihara, Osamu Miura, Kozo Konishi, Sachiko Takeo, Tadatoshi Kakimoto, Gen Hidaka, Yuichi Shibui, Yoshikazu Minamisono, Tomohiro Toda, Shuichiro Uemura, Masakazu Yamamoto, A case of postoperative recurrent cholangitis after pancreaticoduodenectomy successfully treated by tract conversion surgery, Journal of Surgical Case Reports, Volume 2016, Issue 7, July 2016, rjw123, https://doi.org/10.1093/jscr/rjw123
Close - Share Icon Share
Abstract
A 69-year-old man, who had undergone pylorus-preserving pancreaticoduodenectomy (PD) (Imanaga procedure) for duodenum papilla cancer 13 years prior, had a history of repeated hospitalization due to cholangitis since the third year after surgery and liver abscess at the 10th year after surgery. Gastrointestinal series indicated no stenosis after the cholangiojejunostomy. However, reflux of contrast media into the bile duct and persistence of food residues were observed. We considered the cholangitis to be caused by reflux and persistence of food residues into the bile duct. So, we performed the tract conversion surgery, Imanaga procedure to Child method. The postoperative course was good even after re-initiating dietary intake. He was discharged on the 19th day after surgery. He has not experienced recurrent cholangitis for 18 months. For patients with post-PD recurrent cholangitis caused by reflux of food residues like ours, surgical treatment should be considered because tract conversion may be an effective solution.
Introduction
Cholangitis is one of the potential long-term complications of pancreaticoduodenectomy (PD). Some authors reported that cholangitis was observed postoperatively 5–18% of the cases. Our patient experienced recurrent cholangitis and liver abscess after undergoing pylorus-preserving pancreaticoduodenectomy (PPPD) for duodenum papilla cancer. We report the case of a patient who underwent tract conversion surgery (Imanaga procedure to Child method) at the 13th year after his original surgery, which resulted in a good clinical outcome. To our knowledge, we could find few case reports on tract conversion surgery for treatment of post-PD cholangitis.
Case Report
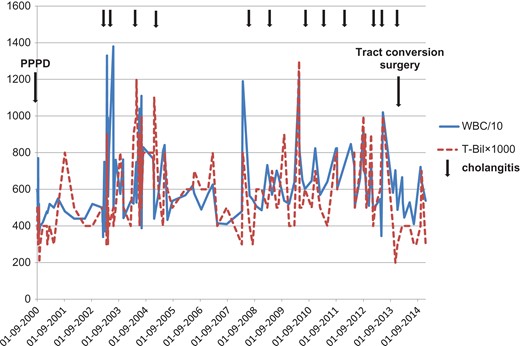
The patient was a 69-year-old man. In 2000, at 56 years of age, he had undergone PPPD (Imanaga procedure) for duodenum papilla cancer. Then, at the third year following surgery, the patient experienced fever several times per year and received conservative treatment for a diagnosis of cholangitis. He also developed liver abscess at the 10th year after surgery (Fig. 1). The patient was hospitalized 12 times in total for cholangitis until the 13th year following surgery. In late June 2013, he developed fever and epigastric pain several hours after dinner and was again hospitalized for suspected cholangitis. His temperature was 38.7°C. White blood cell count was 6.94 × 104/μl, aspartate aminotransferase, alanine aminotransferase, γ-glutamyl transpeptidase were within normal limits. Alkaline phosphatase, total bilirubin and C-reactive protein were mildly elevated to 328 U/l, 1.1 mg/dl and 4.19 mg/dl. Pneumobilia was observed on abdominal ultrasonography. Symptoms were immediately improved by fasting, antibiotics and conservative therapy with fluid replacement.
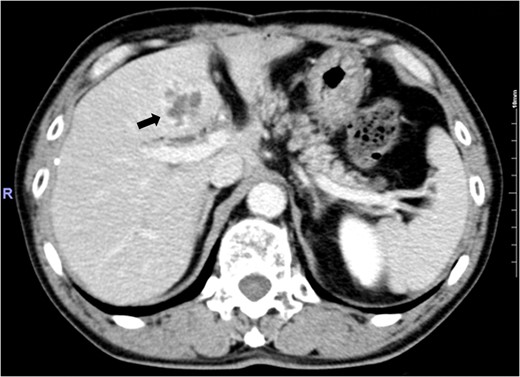
Abdominal enhanced computed tomography image showing an irregular ring-enhanced lesion in Segment 4 of the liver.
Gastrointestinal series showed that contrast media was injected into the bile duct with the patient in a supine position and was visualized; the presence of food residues in the bile duct was confirmed with the patient in a standing position. There was no stenosis associated with choledochojejunostomy (Fig. 2: a, supine position; b, standing position). Thus, reflux and persistence of food residues from the jejunum to the bile duct were strongly suspected as a cause of the recurrent cholangitis. In June 2013, the 13th year after surgery, tract conversion was performed.
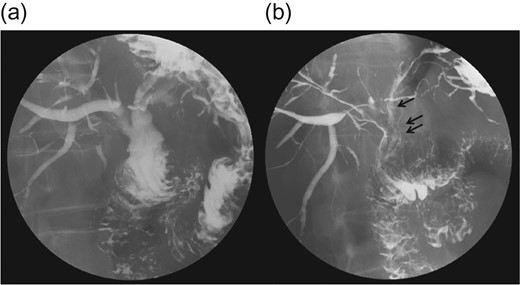
(a) A gastrografin study with the patient in a standing position shows influx of gastrografin to the bile duct. (b) A study with the patient in a supine position shows food debris in the bile duct. The stricture at the anastomosis was not visible.
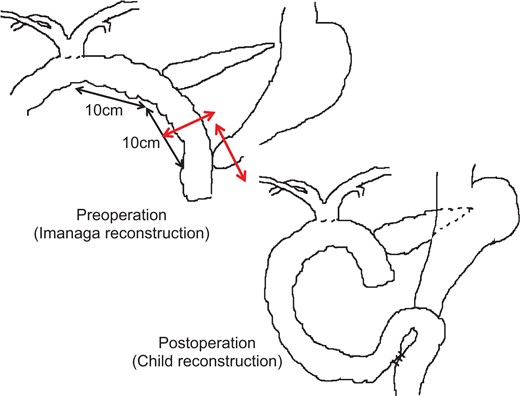
Reconstruction in original surgery had been performed by an antecolic route, using Imanaga procedure. There were ~10 cm separating the gastrojejunostomy, pancreaticoenteric anastomosis and cholenteron anastomosis. The jejunum was resected at the midpoint between the gastrojejunostomy and pancreaticoenteric anastomosis, and a pancreaticobiliary margin was formed. The gastrojejunostomy region was resected and reconstructed in the elevated jejunum using the Billroth II method. Broun anastomosis was added afterwards (Fig. 3).
The postoperative course was good, he was discharged on the 19th day after surgery. Postoperative oral gastrointestinal imaging series revealed limited contrast media inflow into the bile duct. The patient has not experienced recurrent cholangitis in the 18 months following the revision surgery (Fig. 4).
Discussion
The postoperative complications of PD includes pancreatic leak and delayed gastric emptying in the early stage and cholangitis, malnutrition and impaired glucose tolerance in the later stage [1, 2]. Cholangitis is frequently reported (5–18% of cases). Conservative therapy such as fasting and administration of antibiotics is commonly performed. In some patients with severe cholangitis, sepsis due to acute obstructive suppurative cholangitis may occur and may be complicated with liver abscess [2]. Biliary tract infection after reconstructive surgery of the biliary tract is thought to be associated with anastomotic stenosis, malformation of the bile duct located at the side of the liver from the anastomotic site, impaired reconstructed intestinal tract and reflux of food into the biliary tract. Of these, anastomotic stenosis is the most common, generally caused by tumor recurrence or postoperative cholerrhagia. In contrast, obstruction due to postoperative adhesions and cholestasis in the intestinal tract are considered the most common cause of cholangitis following intestinal tract reconstruction [3]. Regarding reflux of foods into the biliary tract, it has also been reported that patients without anastomotic stenosis do not develop cholangitis [4].
Reconstruction of PD includes Imanaga procedure, Cattell, Whipple and Child method. The complications and patient quality of life of these methods have been examined previously [5, 6]. There are several reports on biliary system infection and reconstruction methods [7]. Imanaga procedure is thought to function as follows: as foods pass the upper jejunum, it promotes secretion of enteric hormone and improves digestion and absorption function; as there is no food retention around the anastomotic site, there are limited pancreatic juices or biliary congestion. But then, the incidence of delayed gastric emptying in the postoperative early stage is higher on Imanaga procedure [4]. Some authors reported cholestasis to be more significant and the rate of biliary system infection higher in Child method compared to those in Imanaga procedure [7]. However, previous studies have also reported that gastrointestinal sequence does not have a significant effect on the incidence of cholangitis [8]; thus, there has not yet been a definitive conclusion.
To our knowledge, PubMed database contains no previous reports on tract conversion surgery for the treatment of post-PD cholangitis. Japan Medical Abstract Society website contains few reports on tract conversion for cholangitis [9, 10]. Those described converting from Imanaga procedure to Child method reconstructions and determined the cause of recurrent cholangitis to be reflux of food into the bile duct. In our patient, contrast media flowed easily into the bile duct before reconstruction, and food residues persisted in the bile duct even when the patient was moved to a standing position. After reconstruction, the inflow of contrast media decreased significantly; thus, the possibility for food residues to flow into the biliary tract also decreased. There has been no postoperative development of cholangitis; thus, we believe that the conversion of Imanaga procedure to Child method reconstructions was effective. However, because cholangitis due to cholestasis may occur in the future, careful follow-up is necessary.
Conclusions
Treatment of post-PD recurrent cholangitis requires assessment based on individual clinical conditions, and surgical treatment like that performed in our case should also be considered.
Author's contributions
M.S. contributed in writing the paper. O.M. and S.U. were the attending physicians of the present patient. M.S., O.M. and M.Y. conceived the design and analysis of the case, drafted the manuscript. K.K., S.T., T.K., G.H., Y.S., Y.M. and T.T. participated in design of this case presentation. All authors read and approved the final manuscript.
Conflict of interest statement
None declared.



