-
PDF
- Split View
-
Views
-
Cite
Cite
Manisha Chhetry, Basudeb Banerjee, Shanti Subedi, Ashok Koirala, Necrotizing fasciitis of anterior abdominal wall following cesarean section in a low-risk patient, Journal of Surgical Case Reports, Volume 2016, Issue 7, July 2016, rjw122, https://doi.org/10.1093/jscr/rjw122
Close - Share Icon Share
Abstract
We report a case of a mono-microbial post-cesarean necrotizing fasciitis caused by methicillin resistant Staphylococcus aureus, in a low-risk healthy woman who presented with acute fulminant infection, sepsis and features of multi-organ dysfunction syndrome on sixth post-operative day. Aggressive management with multiple surgical debridement and supportive therapy was the key to favorable outcome in this case.
Introduction
Necrotizing fasciitis (NF) is a severe infection of the skin, subcutaneous tissue and superficial fascia, which has a fulminant course and a potentially fatal outcome [1, 2]. Early diagnosis and surgical intervention can reduce the morbidity and mortality associated with the condition. The lack of early path-gnomonic signs makes it a diagnostic challenge. Usually, the risk factors associated with this condition include diabetes, anemia, malnourishment, intravenous drug abuse and immunosuppressive state [3, 4]. Surgery itself is an independent risk factor. Use of non-steroidal anti-inflammatory drugs in early post-operative period has also been reported as a risk factor in some cases [5, 6].
Few cases of NF have been reported in the obstetric population. Here, we report a case of NF in a post-cesarean patient with no known risk factors, which was managed aggressively with surgical debridement and supportive therapy.
Case Report
A 27-year-old G2P1L1 at 39 weeks period of gestation with previous vaginal delivery was taken up for cesarean section for fetal distress. She delivered a healthy male baby with 3 kg birth weight and mother was discharged on third post-operative day. She presented again on sixth post-operative day with discharge from the wound site with excruciating pain, difficulty in breathing and abdominal distension. At the time of admission, the patient was ill looking, febrile, tachypneic and tachycardic. Her temperature was 100.5°F, blood pressure 120/70, pulse rate 140/minute and respiratory rate of 44/minute. On local examination, the skin around the incision site was edematous, indurate and ecchymosed with suture in situ (Fig. 1). There was sloughing of wound and copious discharge. The abdomen was soft and non-tender, there were right basal crepitations. Her counts were slightly raised (18 000/µl), hemoglobin was 9 gm%, serum creatinine was high (2.3 mg/dl), CRP (C reactive protein) was elevated and serum RBS (random blood sugar) was normal. Ultrasound done showed clumped bowel loops with thickened and edematous wall with thickened omentum and mesentery. The Laboratory Indicator for Risk of Necrotizing fasciitis (LIRNEC) score was 5.
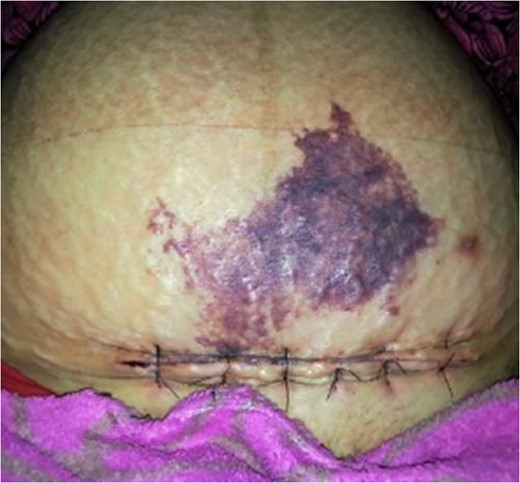
Patient at the time of presentation on sixth post-operative day.
A clinical diagnosis of NF was made and in view of features of sepsis and MODS (multi-organ dysfunction syndrome) she was shifted to ICU and broad spectrum antibiotics started in the form of piperacillin tazobactum and clindamycin. One unit of whole blood was transfused. The patient was taken for surgical debridement (Fig. 2). The rectus sheath was grayish and necrotic with absence of bleeding. There was clumping of the bowel and omentum around the necrotic area. Debridement was done under spinal anesthesia and wound left open (Fig. 3). Pus culture showed methicillin resistant Staphylococcus aureus (MRSA) and antibiotic revision was done with addition of amikacin. Diagnosis was confirmed histopathologically. The patient was kept on intravenous fluids initially and after 72 hours feeds were started and it was gradually built up and she was eventually shifted to high protein diet. As the patient refused skin grafting, regular dressing was done and re-suturing was done on 35th day and at discharge her condition was significantly improved (Fig. 4).



Discussion
NF is a rapidly progressing disease causing extensive soft tissue necrosis commonly involving the limbs, perineum and anterior abdominal wall. Post-operative patients account for 20% of cases, though in many the infection follows trivial trauma.
Most of the cases of post-operative NF in obstetrics and gynecology have been reported before the era of prophylactic antibiotics [7]. Only few cases have been reported after 2000, the latest reported in 2012 by DeMuro et al. [5]. In most of the previous studies obesity, hypertension and diabetes have been implicated as risk factors [7] but recent case reports [5, 6] have highlighted the possible role of post-operative NSAID (non steroidal anti-inflammatory drug). But it is unclear whether it masks the signs and symptoms of NF or actually cause NF [5, 6]. We are of the opinion that NSAIDs delay the diagnosis rather than causing NF as they are routinely used for post-operative pain management.
Bacteriology of the infection was mono-microbial with MRSA isolated from wound swab and it was consistent with the Type II variety of NF usually seen post-childbirth. This type has a more aggressive course with rapid systemic deterioration [8]. The LIRNEC score for this patient was 5; scores more than 8 usually show a good positive predictive value for diagnosis of NF [9]. Low scoring may be due to the routine prophylactic antibiotic therapy given in cesarean patients.
Aggressive and multiple surgical debridement despite patient's unstable condition should be done as there is no role of wait and watch policy. Leaving the abdomen open as in this case, timely performed serial debridement followed by delayed secondary closure with good supportive treatment where the key to favorable outcome. Individualization of therapy should also be done to address specific risk factors like malnutrition and anemia. Though we could not find any specific risk factors in our patient, we are of view that surgery itself was a risk factor in our case.
NF in post-partum patients is a challenge from both diagnosis and management perspective. High clinical suspicion and aggressive management are the foundation for favorable outcome.
Acknowledgement
We would like to thank Dr Yogendra Gupta for editing the final document.
Conflict of interest statement
None declared.



