-
PDF
- Split View
-
Views
-
Cite
Cite
Kendall R. McEachron, Wolfgang B. Gaertner, Extradural sacrococcygeal subcutaneous ependymoma misdiagnosed as pilonidal disease: case report and review of the literature, Journal of Surgical Case Reports, Volume 2016, Issue 7, July 2016, rjw121, https://doi.org/10.1093/jscr/rjw121
Close - Share Icon Share
Abstract
Ependymoma is a type of glial tumor that arises from the ependymal lining of the ventricular system of the central nervous system. These tumors may present as a rare extraspinal variety at the sacrococcygeal region, and may be misdiagnosed as pilonidal disease in the post-sacral area or present with mass-effect symptoms on the bowel or bladder in the pre-sacral region. This is a case of soft tissue swelling at the post-sacral area that, after clinical examination, was diagnosed as pilonidal disease. Surgical excision and pathologic examination revealed a subcutaneous sacrococcygeal ependymoma.
INTRODUCTION
Ependymoma is a type of glial tumor that arises from the ependymal lining of the ventricular system of the central nervous system [1]. These tumors are most commonly seen in children and account for 10% of all CNS tumors [1], and 2–6% of glial tumors [2]. Ependymomas occur in the brain or the spinal cord (more common in adults) [2], and may also present as a rare extraspinal variety at the sacrococcygeal region, separated from the spinal cord. This rare presentation is thought to originate from a group of heterotopic ependymal cells called the coccygeal medullary vestige [3]. Extraspinal ependymomas are further classified by their location relative to the sacrum, and may be misdiagnosed as pilonidal disease at the post-sacral area or present with mass-effect symptoms on the bowel or bladder when located at the pre-sacral region [4]. This case describes the presentation of an extradural sacrococcygeal subcutaneous ependymoma that was misdiagnosed as pilonidal disease. The discussion also includes a current review of the literature on this rare tumor.
VIGNETTE
An otherwise healthy 32-year old woman presented to colorectal surgery clinic with a 1-year history of slow but progressive swelling near her gluteal cleft. The patient denied fevers or chills, increased pain, drainage, bleeding, or rectal bleeding.
On physical exam, there was a 4×4 cm2 area of swelling just left of the natal cleft, at the outer portion of the left perianal skin at the level of the tip of the coccyx. There was mild blanching erythema at the skin overlying the mass; however, there was no evidence of fluctuance or purulence, and no pilonidal pits were visible. Given the high suspicion for abscess, percutaneous aspiration was performed in clinic but no fluid or purulence was obtained. The differential diagnosis at this time included inclusion cyst and soft-tissue tumor. The patient was scheduled for excision in the operating room with no further biochemical or radiographic testing.
In the operating room and under general anesthesia, the patient was placed in prone jack-knife position. A 6-cm vertical incision was placed at the site of the mass, 4-cm left of the midline. A complex and septated 6 × 4 × 4 cm3 mass was excised from the soft tissues at the outer portion of left posterior perianal region, near the coccyx. A rim of healthy-appearing subcutaneous tissue was excised with the mass and care was taken to not rupture or excessively manipulate the mass. The mass was adherent to the subcutaneous fat but there was no involvement of the coccyx or anal sphincter. The mass was anatomically oriented with sutures and sent for permanent pathology. The wound was closed primarily and the patient recovered without complications.
Final pathology revealed a moderately cellular neoplasm with cellular processes extending around blood vessels, formation of perivascular pseudorosettes, and areas of myxoid degeneration (Fig. 1). The neoplastic cells were strongly positive for glial fibrillary acidic protein (GFAP), CD-99, and CD-56, all of which supported the morphologic diagnosis of ependymoma (Fig. 2). The cephalad margin was positive for tumor. A follow up magnetic resonance (MR) of the pelvis and neuraxis was obtained, which demonstrated post-surgical changes and no evidence of persistent tumor (Fig. 3). After evaluation by neurosurgery, full neuro-axial imaging was performed and did not show any evidence of tumor or additional pathology. Excision of the positive cephalad margin and adjuvant chemotherapy or radiotherapy was not recommended. Long-term surveillance with frequent clinical examinations and pelvic MR was established.
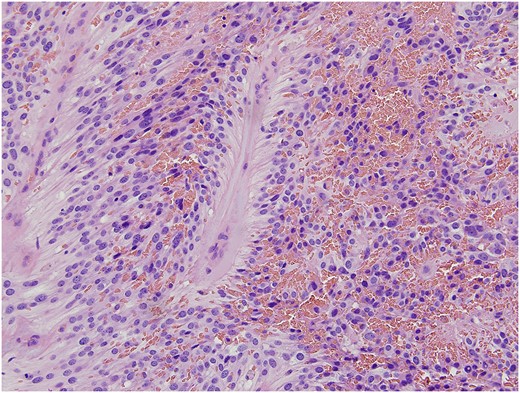
Classic morphologic features of ependymoma including moderately cellular neoplasm composed of cells with mildly pleomorphic round and oval nuclei in a fibrillary background. The neoplastic cells arranged as solid sheets and cords of cells with occasional cribriform pattern. The eosinophilic cellular processes extended around blood vessels with formation of perivascular pseudorosettes. Areas of myxoid degeneration, necrosis and hemosiderin deposition was evident.
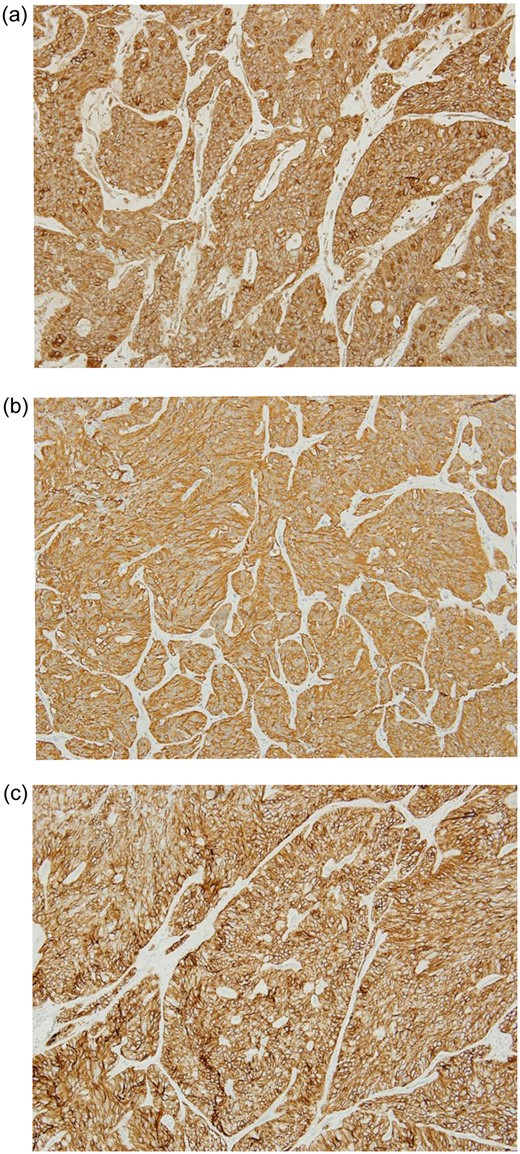
Immunohistochemical analysis demonstrated diffuse and strong expression of CD99 (a), GFAP (glial fibrillary acidic protein) (b), and CD56 (c) in the neoplastic cells. They were negative for cytokeratin (AE1/AE3) which confirmed the morphologic diagnosis of ependymoma.
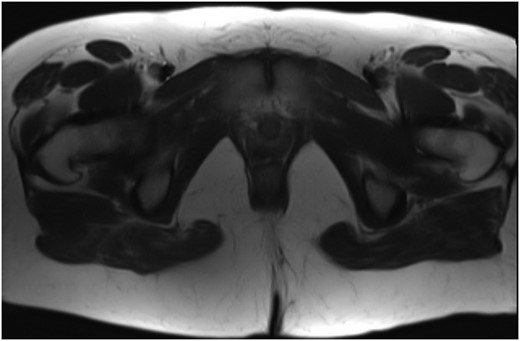
MR of the pelvis showing no evidence of persistent or recurrent sacrococcygeal ependymoma.
DISCUSSION
Extradural sacrococcygeal subcutaneous ependymomas are extremely rare. The first case in the literature was reported by Mallory in 1902 [5]. Ependymomas are classified into three subtypes: myxopapillary, papillary, and subependymal [6]. The majority of subcutaneous sacrococcygeal ependymomas have myxopapillary histology [7], and are located near the gluteal cleft, which leads to a common misdiagnosis of pilonidal disease [4, 8, 9]. These tumors are slow growing and can grow to a large size prior to becoming symptomatic [6, 8]. Of the cases of subcutaneous sacrococcygeal ependymomas reported in the literature, patient age of presentation varies widely from 2 months to 67 years [2–10]. Recommended treatment of subcutaneous sacrococcygeal ependymoma is wide local excision with negative margins [3]. Pathologic examination will demonstrate positive immunohistochemistry for GFAP and S-100 [6–8]. In cases of margin-positive disease, radiation has been reported helpful in several case studies [2, 3, 7], however, chemotherapy seems to be futile [3, 7, 8]. Potential for recurrence in the form of metastatic disease can continue 20 years from the time of primary tumor, so prolonged surveillance is important [2, 7–9].
Author Contribution
Kendall McEachron: contributed significantly to the analysis and interpretation of data, drafting, revising, and final approval, and is accountable for all aspects of this work.
Wolfgang Gaertner: contributed significantly to conception, design, acquisition, analysis, interpretation, revision, final approval, and is accountable for all aspects of this work.
Conflict of Interest Statement
None declared.



