-
PDF
- Split View
-
Views
-
Cite
Cite
Túlio F. Leite, Carlos A.A. Chagas, Lucas A.S. Pires, Rafael Cisne, Márcio A. Babinski, De Garengeot's hernia in an 82-year-old man: a case report and clinical significance, Journal of Surgical Case Reports, Volume 2016, Issue 7, July 2016, rjw120, https://doi.org/10.1093/jscr/rjw120
Close - Share Icon Share
Abstract
The presence of the appendix within a femoral hernia (FH) sac is known as Garengeot's hernia (GH). We report on current study a rare case of an elderly man with a combined inguinal and Garengeot's hernia and discuss the clinical aspects. An 82-year-old man clinically stable, presented history of pain at the right inguinal region for over a week, without vomit, nausea, fever or any alteration of intestinal or urinary eliminations. Clinical examination revealed a FH and the ultrasonography confirmed the hernia sac. During the surgery, the appendix was recognized within the sac, and then, the patient underwent appendectomy and hernia repair. In conclusion, the presence of the vermiform appendix in a FH sac is rare, thus, requiring knowledge of the surgeon regarding this clinical entity. Prompt diagnosis and appropriate surgical treatment is the key to avoid complications.
Introduction
Femoral hernias (FHs) represent a projection of the sac below the inguinal ligament, through the femoral triangle and may contain omentum, pre-peritoneal fat, small intestine, colon and the appendix [1–3]. Garengeot's hernia (GH) is a rare type of FH that includes the vermiform appendix in its sac, with low frequency about 0.8–1% of cases [2]. Such hernias are more susceptible in women during pregnancy, mainly because of the changes in the abdominal wall, as well as a result of a cecum with high mobility or even an enlarged appendix. In rarer cases, the appendix can be inflamed, which increases death risk [2–5]. This clinical condition requires a diagnostic precision and immediate surgery in order to avoid complications [4, 6]. The current study describes GH in an 82-ear-old man.
Case Report
An 82-year-old male was admitted in the emergency. He was clinically stable, with complaints of pain at the right inguinal region, without nausea, vomit, fever or any alteration in intestinal or urinary eliminations. The physical exam showed a non-pulsatile and hardened swelling with tenderness on the right inguinal region. The left inguinal region showed the presence of a reductible and large inguino-scrotal hernia. The ultrasonography suggested inguinal hernia and laboratorial exams showed no alterations. We performed an inguinotomy. After opening the anterior wall of the inguinal canal, it was not identified the presence of an inguinal hernia, although the swelling was still persistent. Afterwards, we reached the subcutaneous tissue above the external oblique muscle's aponeurosis, going to femoral region. After identification of the mass, the adjacent tissues were dissected (Fig. 1) and for our surprise, we found the vermiform appendix emerging from the femoral canal (Fig. 2). Opting for an appendectomy, we sent the appendix to the pathologic exam. The macroscopic exam showed an appendix with a 6.9 cm in length and with an external diameter of 0.9 cm, which presented a congested serosa, fibrin deposit and a mesoappendix of 2.1 cm. The whitened walls and its lumen had pasty fecal matter. The microscopic exam showed no signs of acute appendicitis or abnormal intraluminal content. Patient was monitored postoperatively for 3 days and was discharged without any complications.

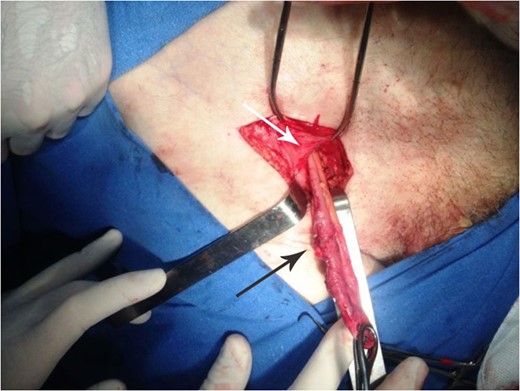
Shows a vermiform appendix (black arrow) within the femoral ring (white arrow).
Discussion
GH is very rare, as it occurs around 0.5–3.3% of FH cases. The first description was in 1731 by Rene Jacques Croissant De Garengeot, a French surgeon [2].
The presence of the appendix in the hernia sac is associated with the anatomical variation of its position, its size, the embryological intestinal rotation, a more mobile cecum or even a larger cecum that invades the pelvic cavity. The hernia sac may contain omentum, pre-peritoneal fat, small intestine loop and colon [1, 3, 7, 8].
The GH, unlike the Amyand hernia—which is found predominantly in men—shows a higher predisposition of happening in women undergoing through the postmenopause period (four women to one men ratio), as a result of a larger femoral canal [5, 8]. It is known that multiparous women possess a higher risk of developing a FH, although men possess a higher risk than nulliparous women [8, 9].
The anatomic display of the femoral canal can induce appendix inflammation. Because of the size and the stiffness of the femoral ring, the appendix suffers external compression, inducing a higher risk of incarceration and strangulation of the hernia. This theory can be explained by the absence of appendicolith: frequent provokers of acute appendicitis, as reported in some cases. Nonetheless, the stiffness of the femoral canal can also be the answer to the fact that it prevents the infection of spreading through the abdominal cavity, averting peritonitis [5].
The symptoms such as fever and bowel obstruction are unspecific, but in severe cases it can evolve to a shock. The differential diagnosis should include inguinal hernia, inflammation of nearby viscera, great saphenous vein ectasia, lipoma or others soft tissue neoplasia, lymphoma and retroperitoneal abscesses [5].
The GH diagnosis is typically done during the surgical act, considering that the clinical-radiologic findings are unspecific. The white blood cell counts and reactive protein C dosage will indicate inflammatory process, the abdomen X-ray should be ordered to exclude small intestine obstruction and the ultrasound is performed with the purpose of identifying the hernia sac content or the presence of liquid. In simpler cases, the diagnosis can be obtained merely with the use of the ultrasound, in which is observed a swollen tubular structure with a ‘dead-end’ lumen adjacent to the right femoral vein [6, 7, 10].
Nevertheless, the best radiologic result is achieved with CT-scan, since it can observe unconfined liquid at the hernia sac, the association of the mesoappendix, incarcerated fat, extraluminal or intramural gas and the precise position of the cecum. In addition, the CT-scan is the best method to distinguish an Amyand hernia from GH [3, 4].
Laparoscopic intervention is the most common treatment, since it is minimally invasive and has a small chance of relapse, although this procedure requires knowledge of the surgeon regarding the myopectineal orifice, also, the surgery requires knowledge about anatomic variations in arteries and nerves of the area, as there are reported cases of aberrant obturator arteries. The obturator artery is usually a branch of the internal iliac artery, but, in rare cases, the obturator artery becomes a branch of the external iliac artery instead, causing it to have a different trajectory: it runs right behind the FH sac, increasing chances of rupture and subsequent hemorrhage [8, 10].
The GH can be associated with complications such as appendicular ischemia, necrosis, perforation, peritonitis or local inflammation, abscess formation, necrotizing fasciitis and intestinal loop obstruction. Those complications should be avoided especially in elder patients, because the evolution of those symptoms can be fatal [6]. Once diagnosed, the indicated treatment for the GH is an appendectomy—if there is appendicitis or perforation—followed by hernia repair. In case of appendicitis, the surgical treatment is enhanced with the association of antibiotics before surgery. The surgical intervention needs to be immediate, as GH can quickly develop into those complications [2, 3, 10].
Fundings
None declared.
Conflicts of Interest
The authors declare no conflicts of interest.
Acknowledgements
None.



