-
PDF
- Split View
-
Views
-
Cite
Cite
Samuel Dobrowolski, Guilherme Lepski, Marcos Tatagiba, Meningioma arising in the hypoglossal canal: the midline suboccipital subtonsillar approach, Journal of Surgical Case Reports, Volume 2016, Issue 7, July 2016, rjw039, https://doi.org/10.1093/jscr/rjw039
Close - Share Icon Share
Abstract
Hypoglossal canal meningiomas (HCMs) are extremely rare, and a consensus has yet to be reached regarding the most appropriate treatment approach for these types of tumors. Surgical procedures to the hypoglossal canal are often complex and lengthy, and are often associated with high rates of morbidity. Several approaches have been used to remove such lesions. Most of these approaches have been adapted from methods used for jugular foramen surgery. Our goal is to present an approach that improves visualization of the hypoglossal canal, thus reducing this pathology's risk of morbidity. In this report, we describe one case of HCM in which the tumor was safely and effectively removed by the midline subtonsillar approach, which allows for a direct primary intradural visualization of the hypoglossal canal. There was no postoperative complication in the patient. The length of follow-up was 73 months, and there has been no recurrence of the tumor.
INTRODUCTION
Meningiomas are common neoplasms affecting the nervous system and represent 19% of all primary intracranial tumors [1]. However, meningiomas, arising in the hypoglossal canal, are extremely rare, with only three cases reported in the literature so far [1–3]. The choice of treatment approach depends on several factors, including tumor type, size, compression of neural structures, patient age, symptoms and co-morbid conditions. Should surgery be considered, there is currently no consensus regarding the ideal surgical approach for treating these lesions [4]. Commonly used approaches for accessing the hypoglossal canal are the lateral transcondylar and far-lateral supracondylar approaches [3, 4].
Here, we report a case of a meningioma that arose in the hypoglossal canal. In our case, the transdural and intradural parts of the tumor were safely removed with a direct primary view to the hypoglossal canal by the midline subtonsillar approach (STA).
CASE REPORT
Our patient was a 45-year-old woman who reported having chronic headaches. The neurological examination revealed no neurological deficits, including normal lower cranial nerve function.
The MRI showed a gadolinium-enhanced extra-axial mass within the right aspect of the foramen magnum. The mass extended from the medulla oblongata to the C1 level of the spinal cord, deforming the right aspect of the upper cervical spinal cord and medulla oblongata. The MRI was complemented by a CT scan and by dynamic cervical spinal X-ray (flexion–extension views; Fig. 1 ).
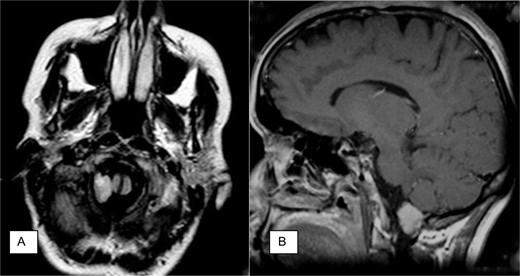
Neuroradiology findings. (A) Axial fast fluid-attenuated inversion recovery (FLAIR) image demonstrates intradural mass at the right foramen magnum resulting in slight displacement of the medulla and transdural hypoglossal canal involvement. (B) Sagittal contrast-enhanced T1-weighted spin-echo image demonstrates intradural mass at foramen magnum.
The mass was excised and found to be a meningioma that had originated from the arachnoid of the hypoglossal canal (Fig. 2). A microscopic examination confirmed the presence of meningothelial cells and abundant psammoma, which resulted in the diagnosis of psammomatous meningioma—WHO grade I. Neither recurrent tumors nor regrowth were observed at the follow-up (73 months) [5].
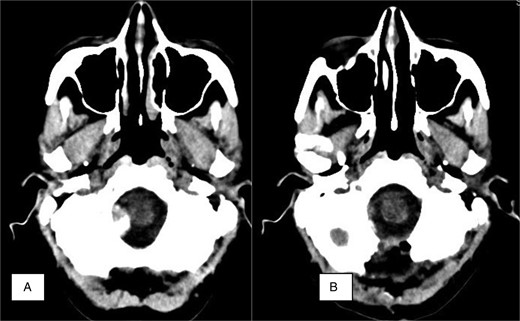
Neuroradiology finding. (A) Axial CT. Preoperative calcified mass at the right foramen magnum resulting in slight displacement of the medulla. (B) Axial postoperative CT showing no residual tumor and bone resection.
During the surgical procedure, an electrophysiologist measures bilateral somatosensory evoked potentials and makes electrophysiological recordings of the ipsilateral VII–XII cranial nerves. The patient is placed in the prone (concorde) position. The head is placed in an antero-flexion position and fixed with the Mayfield (a three pin-type head holder).
A midline vertical skin incision is made from the inion to the second vertebral lamina and a burr hole is made over the external occipital protuberance. The craniotomy is directed toward the foramen magnum, which is open. The posterior arch of the C1 is removed. The dura is opened under the surgical microscope in a Y-like fashion. The tumor is initially debulked up to the brainstem and the lower cranial nerves.
The hypoglossal nerve was sacrificed and the dural attachment to the tumor was coagulated. Although the right vertebral artery was encapsulated and displaced by the tumor, we were able to release the artery through careful microdissection. We performed a macroscopically complete resection with endothermy coagulation of the dural attachment (Simpson II) [6].
DISCUSSION
Transcondylar approaches have been preferred to the removal of hypoglossal schwannoma [7–9]. Far-lateral approaches (with transcondylar and supracondylar variations) are currently used for approaching the anterolateral margin of the foramen magnum. The transcondylar variant is directed above the atlanto-occipital joint through the occipital condyle and below the hypoglossal canal to access the lower clivus [10]. The supracondylar approach is directed above the occipital condyle to the hypoglossal canal or both above and below the hypoglossal canal to the lateral side of the clivus [10]. A direct access to the hypoglossal canal is not given, however, because the angle of view is direct from lateral to medial, while the hypoglossal canal courses obliquely—in a medial-to-lateral direction.
The STA gives excellent access, providing a panoramic view of the foramen of Luschka laterally and up to the middle cerebellar peduncle [4]. However, the STA has not yet been described for resecting meningiomas of the hypoglossal canal although the suboccipital midline approach allows tumor removal through a direct angle of view. In addition, the STA takes into consideration the anatomical displacement commonly caused by the lesion. Radical resection of the lesion—even of its extracranial parts—is feasible with a standard craniotomy, which does not require additional time for bone drilling [5].
CONFLICT OF INTEREST STATEMENT
The authors alone are responsible for the content and writing of the paper.
REFERENCES



