-
PDF
- Split View
-
Views
-
Cite
Cite
Bilal Rafique, Benjamin H. Miranda, Esha L. Gopee, Andrew J. Wigham, Neil J. Toft, Recurrent gluteal haematoma: two internal iliac artery-associated bleeding points, Journal of Surgical Case Reports, Volume 2016, Issue 6, June 2016, rjw107, https://doi.org/10.1093/jscr/rjw107
Close - Share Icon Share
Abstract
Isolated iliac artery aneurysms are extremely rare. Gluteal artery aneurysms are also rare, more commonly affecting the superior gluteal artery in association with penetrating trauma, with those of the inferior gluteal artery usually associated with pelvic fractures. We discuss a diagnostically challenging presentation of recurrent subcutaneous gluteal haematoma due to two separate internal iliac artery-associated bleeding points. A 67-year-old man was referred, from a peripheral hospital, with a right-sided subcutaneous gluteal haematoma. This manifested 28 days following minor non-penetrating, non-fracture-associated trauma. Despite repeat blood transfusions, albeit interspersed with days of haemodynamic stability, and despite exclusion of relevant bleeding sources at endoscopy and two surgical explorations, it was only until contrast CT scanning was requested that both bleeding sources were identified and successfully treated by endovascular coil embolization. This provides an important variant and lesson to supplement current literature and understanding of more diagnostically challenging cases of an extremely rare presentation.
INTRODUCTION
Isolated iliac artery aneurysms are extremely rare, representing only 0.03% of a series of 26 251 autopsy patients, mostly associated with atherosclerosis and with other aetiological factors including trauma and infection [1]. Presentation is variable including incidental findings during surgery, abdominal or rectal examination, acute rupture, ureteric obstruction, sciatic nerve compressive neuropathy or pelvic vein compression [2]. Gluteal artery aneurysms are also rare, more commonly affecting the superior gluteal artery in association with penetrating trauma, with those of the inferior gluteal artery usually associated with pelvic fractures [3, 4]. Although often asymptomatic, presentations may include progressive gluteal swelling, a mass mimicking a gluteal abscess, a tumour or be associated with sciatic nerve compression symptoms [5].
CASE REPORT
A 67-year-old, non-communicative man was referred to plastic surgery with a right-sided subcutaneous gluteal haematoma and low haemoglobin after a minor fall 28 days previously. Despite there being no obvious bleeding points after two surgical haematoma evacuation procedures, interspersed with days of haemodynamic stability, the patient required repeat blood transfusions.
DISCUSSION
On Saturday (day 2), a 500 ml haematoma was evacuated at our institution under general anaesthesia via a 4 cm incision. There were no identifiable bleeding points and he was transfused 2U of packed red cells peri-operatively, increasing his Hb to 8.7 g/dL. The patient was haemodynamically stable, throughout Sunday (day 3), with no clinical features of recurrence. On Monday (day 4), the haematoma recurred and his Hb dropped from 8.7 g/dl to 4.9 g/dl, prompting a second transfusion of 4 units of packed red cells, increasing his Hb back to 8.7 g/dl. On Tuesday (day 5), a further Hb drop to 6.4 g/dl prompted transfusion of 2U of fresh frozen plasma 3U of red cells and surgical haematoma evacuation; however, there was no identifiable active haemorrhage. The patient was haemodynamically stable throughout Wednesday (day 6). Gastroscopy and colonoscopy were performed due to a past medical history of haematemesis; however, no recent/active bleeding was identified.
The patient continued to be haemodynamically stable throughout Thursday (day 7), abdomen and pelvis contrast CT indicated two bleeding sites arising from the internal iliac artery region. One was identified arising from the posterior division of the right internal iliac artery, at the inferior gluteal artery (Fig. 1a). A second, less prominent bleeding point was noted at the division level of the internal iliac artery into its anterior and posterior branches, anterior to the sacroiliac joint (Fig. 1b). Selective angiography was also performed, identifying a large pseudoaneurysm arising from the inferior gluteal artery and endovascular repair was undertaken (Fig. 2). The right common iliac artery was accessed via a left common femoral artery puncture and a combination of five 2 × 5.0 mm Figure 8–18 pushable coils and two VortX™-18 pushable coils of 3 × 2.5 mm and 4 × 4.0 mm respectively (Boston Scientific, Massachusetts, USA) were deployed to embolize the inflow and outflow vessels (Fig. 2). A further 200 mls of blood were evacuated from the right buttock wound post-embolization. Haemostasis was achieved successfully and wound closure undertaken on the following Monday (day 11).
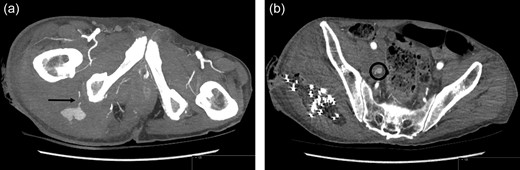
Contrast CT Scan: (a) Inferior gluteal artery haemorrhage. (b) Second site of haemorrhage at the level of division of the internal iliac artery into its anterior and posterior branches, anterior to the sacroiliac joint.

Interventional Angiogram: Deployment of seven coils to embolize the inflow and outflow vessels of the inferior gluteal artery pseudoaneurysm.
We present a diagnostically challenging case of recurrent subcutaneous gluteal haematoma, uniquely associated with 2 bleeding points relating to the internal iliac system. At surgery, no identifiable cause was found. Internal iliac and gluteal artery aneurysms are extremely rare, often traumatic in origin and predominantly classified as pseudoaneurysms [1, 3, 4]. They may be slow-growing and present late either as an incidental finding or with gluteal swelling and bruising, compressive neuropathy or compression of surrounding structures. Differential diagnosis should include a gluteal abscess and gluteal compartment syndrome [5–7]. Radiological investigations including duplex, CT and MRI may facilitate bleeding course identification, shape, size and position relative to surrounding structures. Angiography however is diagnostically invaluable in delineating the anatomy of the arterial branches involved and in facilitating intervention [5, 8].
Aneurysms of the internal iliac artery and branches have a poor prognosis if left untreated. Estimated mortality ranges between 50% and 75%, when in isolation, due to rupture and fatal haemorrhage [1, 5]. Traditional treatment includes open surgical artery ligation both proximal and distal to the aneurysm to minimize recurrence risk due to collateral circulation [6]. Due to the potential difficulty in identifying sites of haemorrhage, such as in our reported case, endovascular angiographic repair using embolization, coils and stents is increasingly replacing open surgery [9, 10]. Although this carries the incontestable advantage of being minimally invasive over surgery, embolization alone may be insufficient for pseudoaneurysm treatment as it is less likely to relieve exerted pressure on surrounding structures, while coils and stents may dislodge and migrate.
This case uniquely reports recurrent gluteal haematoma in a non-communicative patient which manifested 28 days following minor, non-penetrating and non-fracture-associated trauma. Furthermore, although the rare internal iliac artery system pseudoaneurysm has been reported, no similar report exists in the literature with two bleeding sources and with this mechanism of injury. Despite repeated requirements for low Hb associated blood transfusions, albeit interspersed with days of haemodynamic stability, exclusion of relevant history-related bleeding sources, and by endoscopy and two surgical explorations, it was only until contrast CT scanning was requested that two separate bleeding sources were identified and successfully treated by endovascular coil embolization. This report provides an important variant and lesson to supplement current literature and understanding of more diagnostically challenging cases of an extremely rare presentation; it highlights the importance of maintaining a high index of suspicion and investigating the possibility of multiple bleeding points in cases of subcutaneous gluteal haematoma, even when the presentation is several weeks following minor non-penetrating and non-fracture-associated trauma.
Conflict of Interest Statement
None declared.
Sources of Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.



