-
PDF
- Split View
-
Views
-
Cite
Cite
Christina Ble, Parmenion P. Tsitsopoulos, Dimitrios M. Anestis, Sofia Hadjileontiadou, Triantafyllia Koletsa, Maria Papaioannou, Christos Tsonidis, Osteoporotic spinal burst fracture in a young adult as first presentation of systemic mastocytosis, Journal of Surgical Case Reports, Volume 2016, Issue 4, April 2016, rjw063, https://doi.org/10.1093/jscr/rjw063
Close - Share Icon Share
Abstract
Osteoporotic vertebral fractures are uncommon in young adults and usually indicate an underlying disease. Systemic mastocytosis is a myeloproliferative neoplasm, which can be associated with osteoporosis. A previously healthy 30-year-old man presented with an L4 burst fracture after lifting a heavy object. He was operated with laminectomy and posterior lumbar instrumentation. During surgery, abnormally soft bone was noted. Postoperatively, osteoporosis was confirmed with measurement of bone mineral density. Further investigation revealed elevated serum tryptase levels while bone marrow biopsy findings showed systemic mastocytosis. He was also tested positive for D816V KIT mutation. Treatment with biphosphonates and interferon was initiated. No extraskeletal involvement was noted up to the last checkup, 18 months after the first presentation. Abrupt vertebral fractures in apparently healthy young individuals should raise the suspicion of an underlying pathology. Prompt identification and treatment of systemic mastocytosis is crucial in order to avoid unexpected sequelae.
Introduction
Non-traumatic vertebral fractures are infrequently the first symptom of an undiagnosed osteoporosis [1, 2]. Young adults presenting with osteoporosis may suffer from an underlying disease that necessitates meticulous exploration. Systemic mastocytosis constitutes a rare group of disorders characterized by clonal proliferation of mast cells in various organs [1]. Resulting symptoms are related to tissue infiltration, release of mast cells or the presence of an associated hematologic disorder [3].
A case of an osteoporotic vertebral fracture in a young man as the first presentation of systemic mastocytosis is reported.
Case Report
A previously healthy 30-year-old man presented with sudden and intense back pain after lifting a heavy object. Radiological investigation demonstrated an L4 burst fracture with presence of bone fragments in the spinal canal (Fig. 1). Clinical examination was normal except for a mild left foot numbness. His routine laboratory assessment revealed hypochromic microcytic anemia.
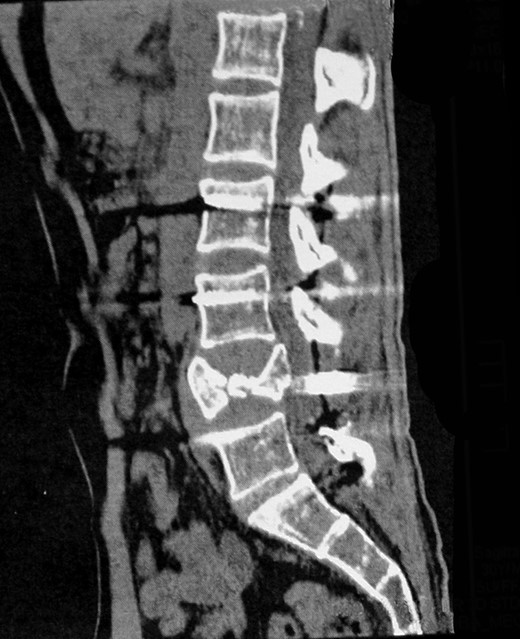
Computed tomography scan of the lumbar spine showing an L4 burst fracture.
He underwent a complete L4 and a partial L3 laminectomy plus posterior lumbar fusion with pedicle screws from L2 to S1 vertebrae. Remarkable vertebral softness was documented during surgery. Postoperatively, bone mineral density was measured and showed osteoporotic findings. The postoperative course was uneventful. Further investigation found abnormally elevated serum tryptase levels: 25.2 μg/l (normal values <11.4 μg/l). Α bone marrow biopsy was performed and showed nests of spindle-shaped or ovoid cells with atypical morphology, eosinophilic cytoplasm and irregular or elongated nuclei. Ηistochemical staining with chloroacetate esterase and Giemsa and immunohistochemical staining with tryptase and CD117 demonstrated similar cell aggregates (Fig. 2). A bone marrow sample tested by polymerase chain reaction was found positive for the D816V somatic mutation in the exon 17 of the c-KIT gene.
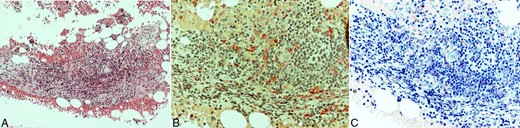
Bone marrow biopsy. Hematoxylin and eosin (H&E) stain showing nodular infiltration by lymphocytes and atypical mast cells, forming loose aggregates (A), highlighted by chloroacetate esterase (B), and Giemsa histochemical stains (C). A, H&E (×200); B, Chloroacetate esterase (×400); C, Giemsa (×400).
These findings established the diagnosis of systemic mastocytosis according to the criteria of the World Health Organization (WHO) [4].
Treatment with biphosphonates and interferon was initiated, which is well tolerated at 18 months following the diagnosis. Over this period, he has not developed any skeletal or extraskeletal signs of the disease. Regular imaging follow-up did not show any instrumentation failure, new vertebral fracture or subsidence and signs of screw loosening (Fig. 3). Soon after surgery, he returned to his normal activities free of pain without any neurological deficits.
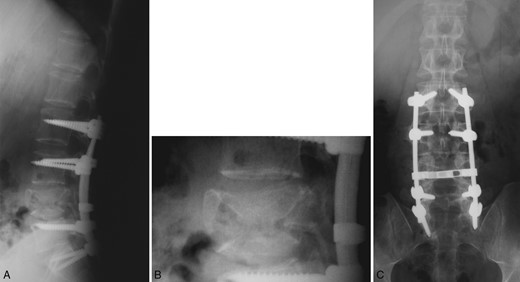
Postoperative plain radiograph of the lumbar spine following L2 to S1 posterior instrumention at 15 months. Good bony fusion is documented at the fractured vertebra with no signs of instrumentation failure.
Discussion
Systemic mastocytosis has long been identified as a potential cause of osteoporosis. However, due to its rarity, only recently had relevant studies on a notable number of patients been conducted [5]. It is characterized by abnormal proliferation and accumulation of mast cells in various organs (most commonly the skin) and release of biological mediators such as histamine, prostaglandin D2, platelet-activating factor, cytokines, leukotrienes, chemokines and tryptase [3]. Clinical manifestations vary depending on the effect of the released mediators on each tissue and the accumulation of mast cells in the tissues [3, 5]. Indolent systemic mastocytosis is defined by the presence of abnormal mast cells outside the skin, principally in the bone marrow [3]. Osteoporosis is the most prevalent bone manifestation; however, osteosclerosis has also been described [5, 6]. Interleukin-1, interleukin-6 and tumor necrosis factor alpha are important regulators of bone resorption, with their serum levels associated with the severity of symptoms and the presence of osteoporosis [5].
In a study of 75 patients with systemic mastocytosis, 31% of the cases were involved with osteoporosis. Lumbar fracture was found in 43% of osteoporotic patients, while 30% suffered from multiple lumbar fractures [6]. Another study investigated the prevalence of lifetime fractures in 157 patients with systemic mastocytosis. Osteoporosis was observed in 28% of cases. Of 140 fractures that occurred in 57 patients, 87 were vertebral [5]. Rossini et al. studied 199 patients with systemic mastocytosis and found a 12% incidence of osteoporosis in males and 33% in females. The incidence of vertebral fracture was 20% in males and 14% in females [7]. However, to our knowledge, the incidence of lumbar fracture as first presentation of systemic mastocytosis has not been previously reported.
The diagnostic WHO criteria for systemic mastocytosis include one major (multifocal dense infiltrates of mast cells in bone marrow or other extracutaneous tissue with confirmation by immunodetection of tryptase or metachromasia) and four minor criteria (abnormal mast cell morphology with a spindle shape and/or multilobed or eccentric nucleus, aberrant mast cell surface phenotype with expression of CD25 and CD2 in addition to C117, detection of codon 816 mutation in peripheral blood cells, bone marrow cells or lesional tissue and total serum tryptase >20 ng/ml). The existence of one major and one minor criterion or the presence of three minor criteria establish the diagnosis of systemic mastocytosis [4]. In the current report, the presence of one major and two minor criteria (detection of KIT point mutation at codon 816 in peripheral blood and serum total tryptase >20 ng/ml) confirmed the diagnosis.
Treatment approach of systemic mastocytosis depends on the clinical presentation of the disease and the severity of symptoms. In cases with prominent bone disease (osteoporosis and/or skeletal fractures), biphosphonates alone or in combination with a cytoreductive agent, such as interferon alpha, are the first-line options [6, 8, 9]. Bisphosphonates increase vertebral bone mineral density around 2% per year and prevent osteoporotic fractures [8]. If interferon intolerance becomes an issue or in severe cases where the disease is refractory to interferon, 2-CdA (a purine analog) could be a second-line option [10].
The present case is particularly significant not only due to the absence of any extraskeletal manifestation of systemic mastocytosis but also for the extent of damage caused to the spine that required major surgery. The uneventful postoperative result and the positive response to medical treatment emphasize the importance of a prompt and in-depth investigation of such cases.
Osteoporosis and consequent fragility lumbar fractures are not unusual in patients with systemic mastocytosis. However, extended spinal damage is uncommon and requires aggressive treatment. Therefore, systemic mastocytosis should be included in the investigation of young adults with osteoporotic vertebral fractures despite the absence of clinical symptoms relevant to this disease. Prompt identification and guided treatment of this disease are important to prevent undesirable sequelae.
Conflict of interest statement
None declared.
References
- osteoporosis
- mutation
- bone mineral density
- bisphosphonates
- health evaluation
- interferons
- laminectomy
- lifting
- myeloproliferative disease
- surgical procedures, operative
- pathology
- spinal fractures
- surgery specialty
- burst fracture
- human leukocyte interferon
- mastocytosis, systemic
- bone marrow biopsy
- young adult
- serum tryptase



