-
PDF
- Split View
-
Views
-
Cite
Cite
John M. Ruggero, Shivana N. Prakash, Symptomatic lymphoepithelial cyst of the pancreas: successful treatment without pancreatic resection, Journal of Surgical Case Reports, Volume 2016, Issue 4, April 2016, rjw061, https://doi.org/10.1093/jscr/rjw061
Close - Share Icon Share
Abstract
Lymphoepithelial cysts (LECs) of the pancreas are rare benign lesions with unknown pathogenesis. LECs are true cysts that mimic pseudocysts and cystic neoplasms making diagnosis challenging. We report a case of a symptomatic LEC of the pancreas in a 67-year-old man who had severe epigastric pain. Workup including computed tomography and endoscopic ultrasound were non-diagnostic. The patient underwent attempted surgical resection; however, the mass was unresectable. The mass was enucleated and drained, and pathology returned LEC. The patient underwent a normal postoperative course and remained symptom free. Most LECs are diagnosed after an extensive pancreatic resection for suspicious cystic masses. The aim of this report is to show that operative management of LECs should not be limited to pancreatic resections. Excision and enucleation of LEC of the pancreas is a better alternative than an extensive pancreatic resection. Preoperative diagnosis of LECs appears to be the limiting factor.
Introduction
Cystic lesions of the pancreas are rare [1, 2]. They can be classified into true cysts, pseudocysts and cystic neoplasms. In adults 85–90% of pancreatic cystic lesions are pseudocysts [2]. Lymphoepithelial cysts (LECs) of the pancreas are rare lesions comprising only about 0.5% of all cystic lesions of the pancreas [3]. Luchtrath and Schriefers first described LECs in 1985, and the term LEC was first proposed in 1987 by Truong and colleagues. LECs can mimic pseudocysts; however, LECs are true pancreatic cysts as they are lined by stratified squamous epithelium and surrounded by mature lymphocytes [4]. Previous literature reviews and case series have shown that LECs most commonly occur in middle-aged men, and are asymptomatic or present with nonspecific symptoms. The most common presenting symptom is abdominal pain. Anorexia, fever and weight loss were also common presenting symptoms. The mechanism and pathogenesis of LECs are not fully understood making their initial preoperative diagnosis difficult. In this article, we report a case of a symptomatic LEC that was unable to be successfully diagnosed preoperatively.
Case Report
We present a case of a 67-year-old male with sudden-onset epigastric pain. Medical history was significant for Stage IB non–small-cell carcinoma of the lung, status post resection with adjuvant chemotherapy. The patient had been receiving yearly follow-up imaging, and a pancreatic mass was discovered on follow-up computed topography (CT). The patient was then referred to gastroenterology for an endoscopic ultrasound (EUS). At that time, the mass measured 2.4 cm. The EUS biopsies were non-diagnostic, and the patient was scheduled for follow-up imaging.
Before the follow-up CT, the patient presented to the emergency department with intractable abdominal pain. Initial vital signs and laboratory findings were normal. His physical examination showed significant epigastric tenderness. An abdominal CT showed that the pancreatic mass had doubled in size. There also appeared to be air present in the mass making a pseudocyst or abscess more likely (Fig. 1). Gastroenterology performed a repeat EUS that was again non-diagnostic.
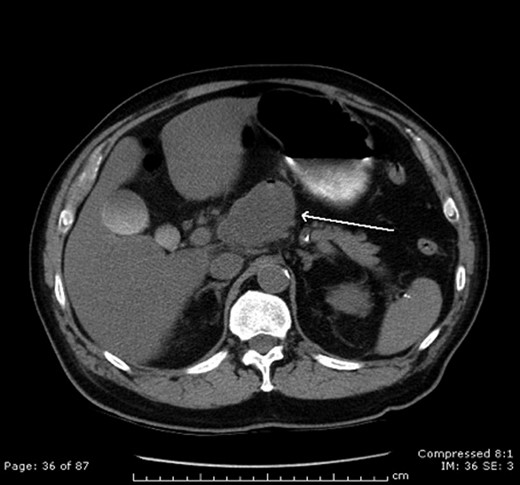
CT scan demonstrating LEC. Note the air present in the cystic mass.
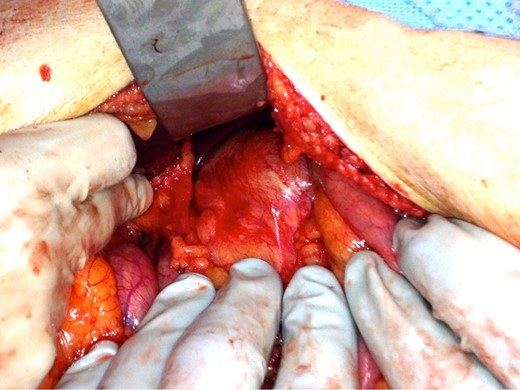
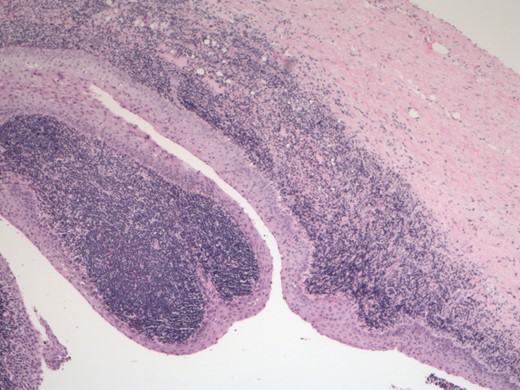
Secondary to the patient’s uncontrolled pain and new CT findings, an exploratory laparotomy was then performed. The mass was found to be adherent to the underlying vasculature, making complete resection impossible (Fig. 2). Given the mass was cystic, it was unroofed, drained and sent to pathology. This revealed a benign LEC of the pancreas (Fig. 3). The patient had an uneventful postoperative course and was discharged home on postoperative Day 6. At 2-week follow-up, the patient was pain free and doing well.
Discussion
LECs of the pancreas are extremely rare. Luchtrath and Schriefers first described LECs in 1985, and the term LEC was first proposed in 1987 by Truong and colleagues. The etiology of these lesions remains unknown. However, some theories previously described include origination from squamous metaplasia of an obstructed pancreatic duct, from the misplacement and fusion of a brachial cleft during embryogenesis or from benign epithelial inclusions or ectopic pancreatic tissue in a peripancreatic lymph node [5].
Adsay et al. reported 12 cases and reviewed a total of 64 cases. Their review showed there is a male predominance (4:1), with an average age of 55 years at diagnosis. The mean cyst size was 4.6 cm (range 1.2–17 cm). These cysts are reported to be symptomatic in 50% of the cases, with the most common symptom being abdominal pain [6].
Diagnosis of a LEC is challenging. Carcinoembryonic antigen (CEA) CA-19–9, carbohydrate antigen-125, cancer-related antigen 72–4, pS2 and mucin-like carcinoma-associated antigen, as well as fluid viscosity would be expected to be significantly lower in LECs than in mucinous neoplasms. However, case reports to date have produced mixed results. Some case reports had an elevated CA-19–9 in the cyst but absent in the serum [7].
LECs are often round with a well-defined wall that is sharply demarcated from the pancreas and surrounding adipose tissue. The main radiographic finding that may help distinguish LECs is that they are sharply demarcated from the pancreatic tissue. Cyst contents are mostly composed of keratin. The cyst contents display a ‘caseous’ appearance characteristic of keratinaceous debris or may be clear and serous in some cases. Microscopically, LECs are characterized by cysts lined by stratified squamous epithelium and immediately adjacent, dense subepithelial lymphoid tissue that contains lymphoid follicles [6].
Few cases have been reported of diagnosis of LEC prior to operation. Cytology classically shows abundant anucleate squamous cells, multinucleated giant cells, mature lymphocytes on a background of keratinaceous debris and a lack of neoplastic cells [8, 9]. Interpretation of LECs by EUS–FNA is complicated by frequent contamination of the aspirate by tissues acquired by the needle during the procedure, making cystic neoplasm difficult to rule out [10].
No recurrences or progression into lymphoma or carcinoma have been documented in the cases of LECs. Pancreatic LECs are benign lesions that are cured by conservative resection. Therefore, if the tumor can be diagnosed preoperatively, the option of ‘wait and watch’ may be clinically acceptable as opposed to surgical resection. However, in most cases, the possibility of another type of pancreatic cystic neoplasm is difficult to rule out [6]. The difficulty in preoperative diagnosis still leads many LECs to invasive surgical resection. Further investigation into more precise preoperative diagnostic modalities is needed to prevent patients from undergoing invasive and morbid surgical resections of a benign disease process.
In conclusion, we have presented a case of a symptomatic pancreatic LEC. In our case report, the LEC was unsuccessfully diagnosed preoperatively despite CT and EUS. This case demonstrates that operative management of LECs can be successfully performed with enucleation and drainage rather than full surgical resection, which is what has been commonly performed in previous case reports. Ideally, improved preoperatively diagnostic techniques need to be further investigated to prevent an extensive resection for a benign process.
Conflict of Interest Statement
None declared.
Ethical Approval
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Acknowledgements
All authors contributed substantially to this project. All authors involved in this project collectively reviewed and agreed upon the information as presented. Furthermore, all authors reviewed and approved the decision to submit this manuscript for publication.



