-
PDF
- Split View
-
Views
-
Cite
Cite
Simon De Freitas, Caoilfhionn Connolly, Colm Neary, Sherif Sultan, Ductus arteriosus aneurysm presenting as hoarseness: successful repair with an endovascular approach, Journal of Surgical Case Reports, Volume 2016, Issue 4, April 2016, rjw060, https://doi.org/10.1093/jscr/rjw060
Close - Share Icon Share
Abstract
An aneurysm of the ductus arteriosus is a rare finding, particularly in the adult population. These saccular aneurysms arise at the site of an incompletely obliterated ductus arteriosus along the lesser curvature of the aortic arch. Left untreated, it is associated with a high risk of potentially life-threatening complications including rupture, infection and thromboembolism. As a result, surgical correction is recommended. Previously, options were limited to open repair but as endovascular experience grows, novel techniques afford safer and less invasive alternatives. In contrast, neonatal ductus arteriosus aneurysms may regress spontaneously and expectant treatment can be justified. We present the case of a 74-year-old woman who presented with hoarseness secondary to a ductus arteriosus aneurysm; a diagnosis consistent with Ortner’s syndrome. The patient underwent an uncomplicated endovascular repair using the chimney-graft technique.
Introduction
Aneurysms of the ductus arteriosus in adults are rare findings and the true incidence is unknown. Previously, most cases were discovered at autopsy or in those undergoing cardiac surgery for another indication [1]. Widespread use of cross-sectional imaging in the adult population has led to increased diagnosis of this often asymptomatic abnormality. Correction is warranted due to the high risk of potentially life-threatening complications including rupture, thromboembolism and acute fistula formation [2]. In contrast, ductal aneurysms occurring in neonates commonly communicate with the pulmonary artery and thereby exist within a patent ductus arteriosus [3]. Operative mortality in this group is higher and the disease follows a relatively benign course such that serial echocardiography monitoring is the initial approach. In this case report, an elderly woman presented with clinical features of recurrent laryngeal nerve palsy secondary to aneurysmal dilatation of the diverticulum of the ductus arteriosus. We report a successful endovascular repair with good recovery of phonation on follow-up.
Case Report
A 74-year-old woman was referred to our vascular service with a 6-month history of hoarseness of voice and intermittent dry cough. The patient’s medical history included hypertension and gastroesophageal reflux disease. Flexible laryngoscopy demonstrated a foreshortened, lateralised and flaccid vocal fold consistent with unilateral vocal cord paralysis. Subsequent computed tomography (CT) imaging of the neck and thorax revealed a saccular aneurysm in the aortopulmonary window measuring 39 mm (Fig. 1). Digital subtraction angiography confirmed the presence of a ductal aneurysm with a well-defined neck and no intraluminal thrombus (Fig. 2). There was no contrast extravasation into the mediastinum or pulmonary circulation. Following a cardiovascular multidisciplinary meeting, treatment options were discussed with the patient and consensus favoured endovascular repair. The distance from the proximal margin of the aneurysmal neck to the origin of the left subclavian artery measured just under 2 cm and therefore did not meet the manufacturer’s minimal landing zone requirements. To circumnavigate this dilemma, a left subclavian stent graft was inserted with its proximal end parallel to the main thoracic endoprosthesis. The procedure was uncomplicated and repeat imaging revealed widely patent stent grafts with satisfactory positioning and absence of endoleak (Fig. 3). Our patient was discharged home on the second postoperative day. She continued speech and language therapy postoperatively and has made remarkable recovery of phonation, declining any further treatment options for same.
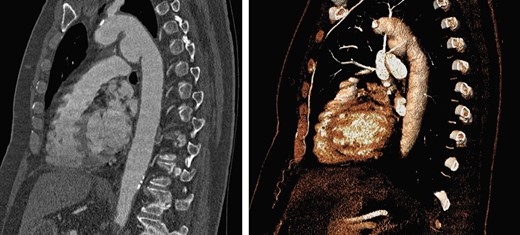
Sagittal CT with 3D reconstruction demonstrated a 39-mm saccular aneurysm along the lesser curvature of the aortic arch, expanding in the direction of the pulmonary artery.
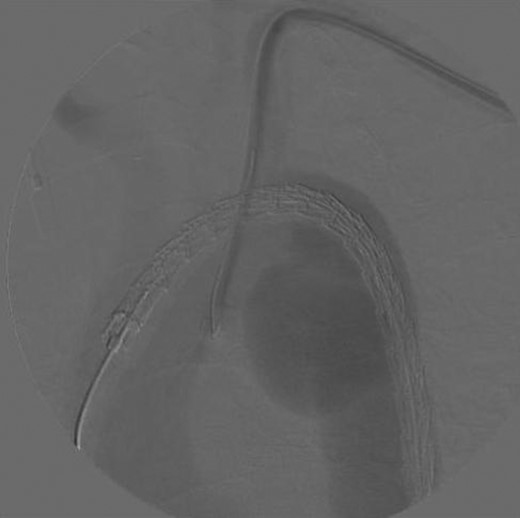
Digital subtraction angiogram demonstrating the chimney-graft approach. Image acquired shortly before simultaneous subclavian and thoracic stent-graft deployment.

Sagittal CT with 3D reconstruction at 1-year post-intervention, showing satisfactory placement of stent grafts.
Discussion
During foetal life, the ductus arteriosus permits ejection of oxygen-rich right ventricular blood into the distal aortic arch, bypassing the high-resistance pulmonary circulation. Following the first breath, the smooth muscle in the ductal walls responds to a variety of biochemical stimuli that promote functional closure [4]. Anatomical closure follows as fibrous tissues proliferate from the pulmonic end of the ductus towards the aorta. Incomplete ductal obliteration at the aortic end gives rise to a diverticular remnant at the posteroinferior aspect of the aortic arch. Subsequently, there is potential for aneurysmal dilatation of the diverticulum with exposure to systemic arterial pressures [5].
Apart from previous repair of a patent ductus arteriosus, risk factors for ductus arteriosus aneurysms have been poorly delineated in the literature. Other associations, but not causal relationships, include connective tissue disorders, chromosomal anomalies and SMAD3 mutations [3, 6, 7]. Of note, our patient sustained blunt chest wall trauma in a road traffic accident approximately 12 years prior to presentation. Sudden deceleration injuries of the thorax commonly cause aortic transection but an association with aneurysmal dilation of the ductus diverticulum has not previously been described. We postulate that remote shearing forces compromised the tunica media at the site of the ductus diverticulum and contributed to aneurysmal dilation.
Our patient presented with a hoarse, breathy voice and intermittent bouts of coughing over 6 months. Laryngoscopic examination demonstrated unilateral vocal cord paralysis consistent with a left recurrent laryngeal nerve palsy. The left recurrent laryngeal nerve passes inferior to the arch of the aorta before ascending in the tracheo-oesophageal groove to supply all the intrinsic muscles of the larynx, apart from the cricothyroid. Therefore, the clinical presentation in this case is consistent with Ortner’s cardiovocal syndrome, in which left recurrent laryngeal nerve palsy arises from cardiovascular disease. In 1897 Norbert Ortner, an Austrian physician, first described three patients with hoarseness of voice secondary to a dilated left atrium in the setting of mitral stenosis [8]. Less commonly reported causes of Ortner’s syndrome include degenerative aneurysms of the aortic arch, dilation of the pulmonary artery, masses in the aortopulmonary window, aortic dissection and iatrogenic injury. Hoarseness in the setting of recurrent laryngeal nerve palsy may be permanent but typically there is some functional recovery as the uninvolved cord develops the ability to hyperadduct and appose the paralysed cord during phonation.
Correction is recommended when aneurysms of the ductus arteriosus are >3 cm, enlarge significantly over time or cause symptoms [2]. In this case, there were two indications for intervention, albeit the most appropriate method of repair was not clearly defined. Given the substantial morbidity associated with open repair, endovascular techniques provide for an attractive, less invasive alternative. However, there are only a small number of reports of ductus arteriosus aneurysms corrected with an endovascular approach [9, 10]. Standard thoracic stent grafts may be used when there is an appropriate landing zone [10]. Otherwise, as illustrated in this unique case, preservation of the left subclavian artery with the chimney-graft technique is possible. Another option would be to perform a hybrid procedure in which a surgical bypass is created before the stent is placed over the left subclavian orifice.
This case highlights the feasibility of a total endovascular approach to complex thoracic aneurysms as an alternative to open surgery. Ultimately, the most appropriate decision should follow multidisciplinary discussion, taking into consideration the expertise of the available endovascular services.
Conflict of Interest Statement
None declared.



