-
PDF
- Split View
-
Views
-
Cite
Cite
Rodrigo C. Surjan, Tiago Basseres, Denis Pajecki, Daniel B. Puzzo, Fabio F. Makdissi, Marcel A.C. Machado, Alexandre Gustavo Bellorio Battilana, A novel technique for hepatic vein reconstruction during hepatectomy, Journal of Surgical Case Reports, Volume 2016, Issue 4, April 2016, rjw054, https://doi.org/10.1093/jscr/rjw054
Close - Share Icon Share
Abstract
Surgical resection is the treatment of choice for malignant liver tumours. Nevertheless, surgical approach to tumours located close to the confluence of the hepatic veins is a challenging issue. Trisectionectomies are considered the first curative option for treatment of these tumours. However, those procedures are associated with high morbidity and mortality rates primarily due to post-operative liver failure. Thus, maximal preservation of functional liver parenchyma should always be attempted. We describe the isolated resection of Segment 8 for the treatment of a tumour involving the right hepatic vein and in contact with the middle hepatic vein and retrohepatic vena cava with immediate reconstruction of the right hepatic vein with a vascular graft. This is the first time this type of reconstruction was performed, and it allowed to preserve all but one of the hepatic segments with normal venous outflow. This innovative technique is a fast and safe method to reconstruct hepatic veins.
Introduction
Surgical resection is the treatment of choice for malignant liver tumours. Recently, there has been a considerable increase in the number of hepatectomies and mortality rates reduced to less than 5% [1]. Nevertheless, surgical approach to centrally located tumours close to the confluence of the hepatic veins is still a challenging issue. Trisectionectomies are considered the first option but are associated with high mortality rates due to post-operative liver failure [2]. Thus, maximal preservation of parenchyma should be attempted.
Recent studies showed that liver parenchymal damage may play a role in tumour cells and their micro-environment [3]. Parenchymal abnormalities that occur during liver regeneration independently worsen oncological outcomes [4–6]. Thus, major hepatectomies with intense post-operative regeneration or segmentectomies that leave parenchyma without adequate venous drainage may not be the best treatment for hepatic malignancies.
We performed a Segment 8 hepatectomy with resection of a segment of the right hepatic vein followed by immediate reconstruction of the vein with a GORE® Hybrid Vascular Graft (W. L. Gore & Associates, Flagstaff, AZ, USA). It allowed to preserve all but one of the hepatic segments and provided optimal venous outflow to remaining segments. This is the first time this technique is performed, and it is a much easier and safer method than other previously reported techniques.
Operative Technique
A 54-year-old male patient with no comorbidities presented with liver metastasis of colorectal adenocarcinoma. He had undergone right hemicolectomy 1 year before and received chemotherapy with FOLFOX followed by bevacizumab.
Computed tomography (CT) disclosed a 4.0 × 2.0 cm lesion in Segment 8 involving the entire circumference of the right hepatic vein (which was still partially patent), extending medially to the middle hepatic vein and posteriorly to the retrohepatic inferior vena cava (IVC) (Fig. 1).
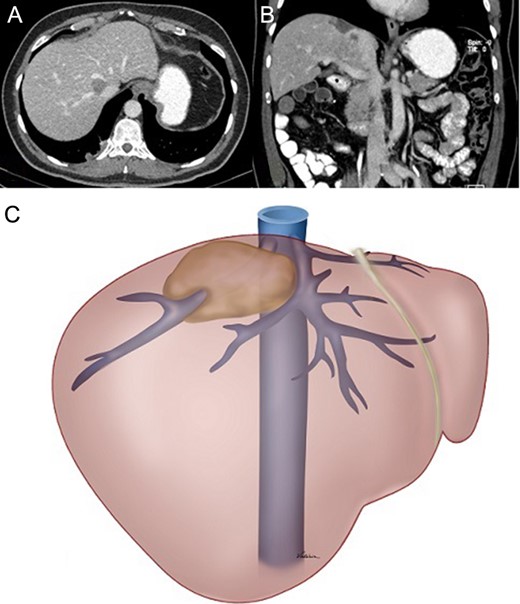
(A) and (B) Preoperative CT showing displacement of the tumour and its relationship with the right and middle hepatic veins and the IVC. (C) Schematic drawing of the tumour.
The idea was to resect Segment 8 with a portion of the right hepatic. As the vein was still patent and there was a concern that a considerable amount of parenchyma could be left with insufficient drainage, we proposed to reconstruct the vein with a graft. The most challenging step of reconstructing the right hepatic vein with a graft is the anastomosis of the graft with the vein in the transected area. We decided to use the GORE® Hybrid Vascular Graft because it allows a sutureless anastomosis at one end of the graft as it has a constrained section with a deployment line that allows easy insertion into the vessel.
A right subcostal incision with an upper midline extension was made. A self-retaining retractor was used. The liver was mobilized by dividing hepatic ligaments.
Intraoperative ultrasound (US) was performed to define tumour margins and its relationship with vascular structures.
The right hepatic vein was dissected through the loose space between the vena cava and the liver and taped.
The parenchyma was transected using bipolar forceps under intermittent Pringle manoeuvre [7]. Transection started at the middle hepatic vein until it was released from the tumour, and proceeded posteriorly to release the tumour from the IVC. Right hepatic vein was cut close to the IVC and the IVC was sutured. The remaining parenchyma was transected and the right hepatic vein was skeletonized for a length of 1 cm to allow graft placement (Fig. 2). Subsequently, the open end of the graft was anastomosed in a standard manner to the IVC (Fig. 3).
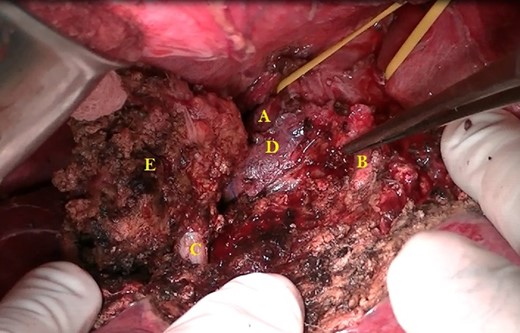
(A) Right hepatic vein sutured close to the IVC. (B) Middle hepatic vein freed from the tumour. (C) Right hepatic vein within the transected area skeletonized for 1 cm. (D) Retrohepatic IVC, area to be anastomosed to one end of the graft. (E) Segment 8 with the tumour.
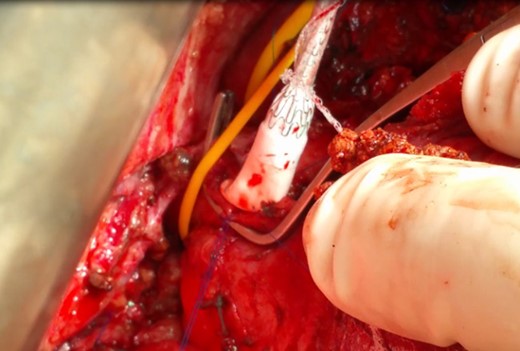
The open end of the graft being anastomosed to the IVC (the graft was previously cut to the proper length, approximately 5 cm).
One last 3-minute Pringle manoeuvre was performed. A venotomy was performed in the right hepatic vein on its skeletonized section. The constrained section of the graft was introduced ~2 cm inside the vein and the deployment line was pulled (Fig. 4).

The right hepatic vein was transected and the specimen retracted. A 19-Fr round Blake drain was placed (Fig. 5). Operative time was 7 hours and estimated blood loss was 100 ml.
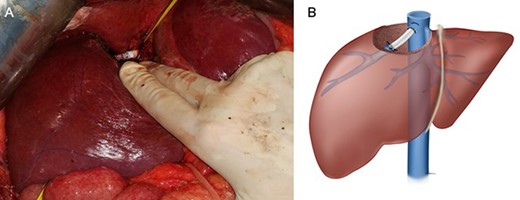
Final appearance: (A) intraoperative appearance and (B) schematic drawing.
Post-operative period was uneventful. Patient spent 1 day on intensive care unit and was discharged from hospital on post-operative Day 6.
Peak aspartate aminotransferase level occurred 5 hours after surgery: 203 U/L (normal range: 15–37 U/L). Patient was discharged with normal aspartate aminotransferase level (32 U/L). Peak alanine transaminase level was 291 U/L at 5 hours after the procedure and 72 U/L at discharge.
Double antiaggregant therapy was initiated on the second post-operative day with clopidogrel (75 mg orally daily) and aspirin (100 mg orally daily). One month after the procedure, clopidogrel was interrupted and aspirin maintained as single-antiplatelet therapy. Doppler US on post-operative Day 2 showed normal blood flow in the graft. Contrast-enhanced CT scans performed on post-operative Day 5 and 3 months after the procedure showed a properly positioned and patent graft (Fig. 6).
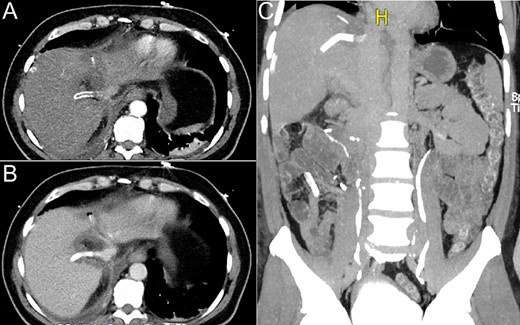
CT scan performed on the fifth post-operative day: (A) axial view, no intravenous contrast; (B) axial view, intravenous contrast inside the graft and (C) coronal view, graft filled with contrast.
Discussion
Hepatectomies have evolved. In recent years, the goal is to preserve as much hepatic segments as possible. However, we are entering a new era, in which not only the liver segments, but also the hepatocytes are the focus of attention. The intention is to produce as little damage as possible to hepatocytes, as liver regeneration may create a micro-environment favourable for tumour cell proliferation and have negative impact on oncological outcome [3–6]. In this context, preservation of hepatic veins is crucial.
Better understanding of the role of the inferior right hepatic vein and that Segment 6 has multiple veins forming numerous anastomoses with surrounding hepatic veins allowed the resection of Segments 7 and 8 including the right hepatic vein without its reconstruction [2, 8–10]. However, atrophy of Segment 6 and liver dysfunction/failure occur in most cases [2, 10].
We decided to resect Segment 8 with right hepatic vein reconstruction using a vascular graft that allowed easy deployment of the graft into the vessel. It ensured maximal preservation of functional parenchyma without congestion, limiting post-operative regenerative activity and parenchymal dysfunction (as judged by low aminotransferase levels), with possible oncological benefits.
Conclusion
Hepatic vein reconstruction is a complex procedure that provides maximal preservation of functional parenchyma. We described a novel technique that allows preservation of liver segments with natural venous drainage, limiting parenchymal dysfunction. It is an easy and reproducible method for reconstructing hepatic veins, which may allow this type of reconstruction to be performed more frequently.
Conflict of interest statement
None declared.



