-
PDF
- Split View
-
Views
-
Cite
Cite
Skyle J. Murphy, Anupinder Kaur, Martin E. Wullschleger, Endometrial decidualization: a rare cause of acute appendicitis during pregnancy, Journal of Surgical Case Reports, Volume 2016, Issue 4, April 2016, rjw053, https://doi.org/10.1093/jscr/rjw053
Close - Share Icon Share
Abstract
Appendicular endometriosis is a rare and poorly understood pathology that affects women in their reproductive years. In the gravid woman, ectopic endometrial tissue undergoes decidualization. This physiological process can result in acute appendicitis in exceptional cases. Here we describe a patient in her second trimester of pregnancy who presented with right iliac fossa pain and clinical, laboratory and imaging findings consistent with acute appendicitis. A laparoscopic appendectomy was performed with intraoperative findings suspicious for malignancy. Histological analysis made the surprising diagnosis of decidualized endometriosis causing luminal constriction resulting in acute appendicitis. We also detail the challenging diagnostic and management issues faced by clinicians in such cases.
Introduction
Endometriosis, defined as the presence of functional endometrial tissue located outside of the lining of the uterine cavity, is a common disorder affecting up to 10% of women of reproductive age [1]. Ectopic endometrial tissue is typically found in the genital tract and pelvic peritoneum [1]. Implantation in the gastrointestinal system is rare, with the prevalence of appendicular endometriosis thought to be <1% [1].
Isolated endometriosis of the appendix is usually asymptomatic. Although, up to one-third of women may experience cyclical right iliac fossa pain [2]. Incidental histological diagnosis following appendectomy is common [3].
During pregnancy, circulating progesterone levels stimulate decidualization of endometrial tissue creating a favourable environment for embryo implantation. This phenomenon is characterized by hypertrophy of stromal tissue, increased glandular secretion and vascular proliferation [4]. Current knowledge suggests that extrauterine deciduas are a benign phenomenon. The natural history of which is atrophy and spontaneous regression resulting in improvement or resolution of symptoms in the post-partum period [4].
Sporadic cases of appendicular decidua reaction resulting in acute appendicitis during pregnancy have been reported in the literature [2, 5–7]. Here we describe such a case.
Case Report
A 31-year-old female (gravida 2 para 1) at 18 weeks gestation presented to the Emergency Department with sudden onset right iliac fossa pain of <12 hours duration. She had associated nausea but no vomiting, fevers, urinary symptoms or per vaginal discharge. The patient had no history of dysmenorrhoea, dyspareunia, subfertility or other gynaecological concerns.
On examination, the patient was afebrile and haemodynamically stable. Abdominal palpation revealed tenderness in the right iliac fossa with voluntary guarding, percussion and rebound tenderness. Neither bimanual nor speculum examination was performed. Blood tests demonstrated leukocytosis (11.6 × 109/L), neutrophilia (8.63 × 109/L; 75%) and mildly elevated C-reactive protein (9.6 mg/L). Beta-human chorionic gonadotropin was appropriate for gestational age (23 000 IU/L). Urine analysis was unremarkable. Ultrasound confirmed a viable intrauterine pregnancy, an inflamed appendix and surrounding free fluid. This was thought to represent acute appendicitis with perforation (Fig. 1).
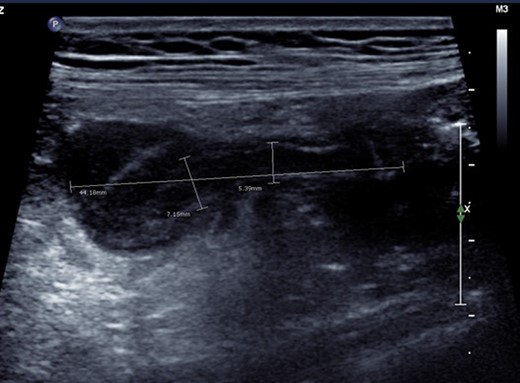
Ultrasonographic appearance of the right iliac fossa. An ill-defined hypoechoic region surrounding a tubular non-compressible structure (maximum calibre 7.15 mm) was identified. This appearance was thought most likely to represent perforated appendicitis with no definable walled-off collection.
During laparoscopic appendectomy, an enlarged appendiceal tip with fibrinous adhesions and haemoserous pericaecal free fluid was seen (Fig. 2). The gross appearance of the appendix was suspicious for appendiceal malignancy (Fig. 3). The appendix was mobilized and transected using endoloops. No other peritoneal or pelvic pathology was identified intraoperatively.
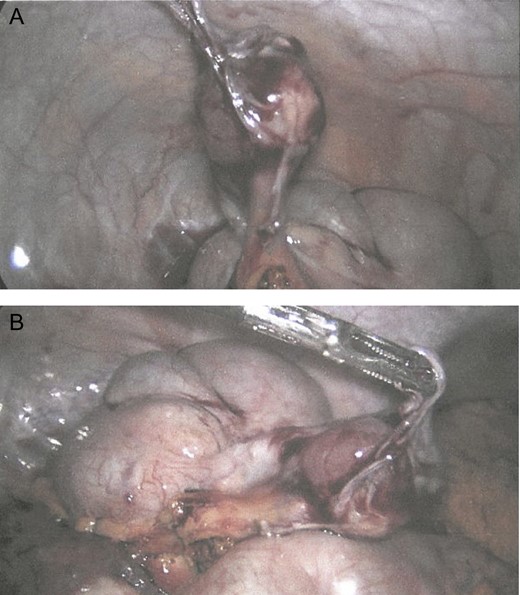
Laparoscopic appearance of the enlarged appendix tip with surrounding fibrinous adhesions and haemoserous free fluid. Appendix base is slim with normal appearance of mesoappendix. A, appendix retracted towards anterior abdominal wall; B, appendix retracted towards the pelvis.
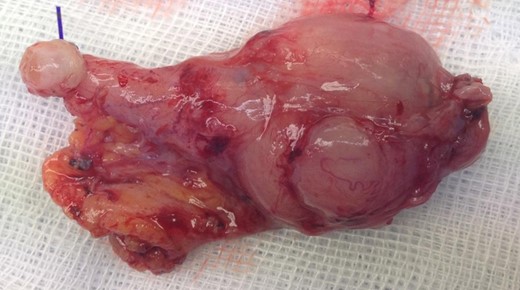
Gross appearance of the appendix following laparoscopic appendectomy. Endoloop in situ base of the appendix. Enlarged appendix tip with fibrinous adhesions lead to intraoperative suspicion of malignancy.
Surprisingly, histopathological examination demonstrated a constricted appendiceal lumen engulfed by decidualized endometriosis (Fig. 4). Invasive endometrial islands were also identified in the submucosa and muscularis propria.
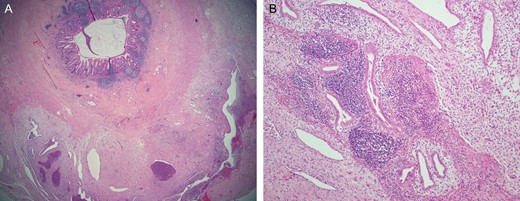
Histopathological appearance of the appendix. Haematoxylin and eosin staining. (A) Low power view of the appendix which was engulfed by and completely surrounded by the endometriosis. (B) Medium power view showing endometrial glands and decidualized stroma.
The patient’s clinical course was uneventful and she was discharged home Day 1 post-operatively. She went on to deliver a live infant via elective repeat lower section caesarean section at 39 weeks gestation.
Discussion
Appendicitis is the most common surgical abdominal pathology encountered in pregnancy, and is responsible for 75% of acute abdomens during pregnancy [1]. Endometriosis presenting as acute appendicitis is estimated to only occur in 3–8 deliveries per 10 000 [5]. In the last 20 years, only four cases of decidualized endometriosis resulting in acute appendicitis have been reported in the literature [2, 5–7].
The pathophysiology of endometriosis is not well elucidated. The most widely accepted theories are retrograde menstruation, haematological dissemination, coelomic metaplasia and autoimmune processes [1]. Ectopic endometrial tissue typically implants in the serosa and subserosa of the appendix, with infrequent involvement of the muscularis and submucosa [2].
Two mechanisms by which decidualized endometriosis produces appendicular inflammation have been described. Fauchereron et al. (2008) posited that volume expansion of endometrial tissue undergoing decidualization causes extrinsic compression of the appendiceal lumen. Conversely, Silvestrini and Marcial (1995) reported intraluminal decidua polyp formation in a pregnant woman with acute appendicitis. The final common pathway of both mechanisms is increased luminal pressure, mucosal ischaemia, bacterial proliferation and inflammation. Importantly, altered antigenicity and increased natural killer cell expression have also been identified in ectopic decidua [3]. This may explain why endometrial appendicitis is associated with higher rates of perforation and abscess formation.
Accurate diagnosis of appendicitis caused by ectopic decidua is exceedingly difficult. As in this case, patients with isolated appendicular endometriosis may not report a pathognomonic history of irregular menstruation, cyclical pelvic pain and infertility [1]. Anatomical and physiological changes associated with the gravid state, including upward displacement of the appendix by the uterus, may result in atypical symptomatology and examination findings. Commonly used laboratory markers of inflammation, including leucocytosis, neutrophilia and elevated C-reactive proteins, are non-pathological findings especially during the second trimester of pregnancy. Ultrasonography is a commonly used imaging modality in the investigation of appendicitis because of its safety and accessibility. Benign deciduae have a heterogenic appearance on ultrasound, which may include increased vascularity and appearance of septations [9]. Sonographic misdiagnosis of pelvic decidua as a more sinister pathology is well documented. In this case, the appendicular decidua was incorrectly identified as free fluid resulting from perforation of the appendix. Because of this positive finding, the treating team opted to proceed directly to the theatre instead of conducting time-consuming magnetic resonance imaging investigation. Diagnostic difficulties associated with appendicular decidua during pregnancy are significant as delayed or inappropriate treatment selection increases maternofetal morbidity and mortality.
Definitive treatment for endometriosis causing acute appendicitis is surgical resection of the appendix. Unlike this case, the majority of appendectomies reported during pregnancy have been performed using laparotomies [10]. Uterine injury, induction of preterm labour and spontaneous foetal demise have been reported in an isolated number of cases [7, 10]. However, a growing body of literature suggests that laparoscopic appendectomy is nowadays a safe and well-tolerated surgical option for pregnant females [10], particularly in the first two trimesters.
Endometriosis of the appendix resulting in acute appendicitis is a rare pathology that is exceptionally difficult to diagnose preoperatively. As this case illustrates, appendicular decidua should be considered as a differential diagnosis for right-sided abdominal pains in the gravid female. The limitations of the current laboratory and imaging techniques in the diagnosis of appendicitis in pregnancy should be recognized. Early intervention is essential with a strong suspicion of appendicitis, in order to prevent perforation and pregnancy-related complications.
Conflict of Interest Statement
None declared.



