-
PDF
- Split View
-
Views
-
Cite
Cite
Dalia Mirjam Gallmann, Kurt-Aurel Stoessel, Othmar Schoeb, Appendicitis after laparoscopic ovarian cystectomy—coincidence or complication, Journal of Surgical Case Reports, Volume 2016, Issue 4, April 2016, rjw052, https://doi.org/10.1093/jscr/rjw052
Close - Share Icon Share
Abstract
Diagnosis of appendicitis, particularly in young women, may be challenging. In case of abdominal pain in the postoperative period of laparoscopic surgery, one should not only think of complications such as bleeding and injury of the bowel but also such as acute appendicitis. We report a case of a 26-year-old female patient with a post-laparoscopic acute appendicitis with appendicolithiasis 3 days after a laparoscopic ovarian cystectomy during which the appendix appeared inconspicuous. Appendicitis after gynecologic laparoscopy is a rare but potentially dangerous condition. One should consider the possibility of a postoperative appendicitis in case of an acute abdomen after laparoscopic surgery. Further studies might be of value to re-evaluate incidental appendectomy especially in cases of appendicolithiasis.
INTRODUCTION
Laparoscopic ovarian cystectomy is a common and safe method for suspected dermoid ovarian cysts [1]. Major complications such as injury of the bowel or the bladder happen in <1% of the cases [1]. Postsurgical fever and small hematoma formation on the abdominal wall at the trocar entries are more common but less severe [1]. The lifetime risk for females for acute appendicitis is 6.7% [2]. Incidental appendectomies used to be performed frequently, but a reversal of trend happened in the 1990s [3].
The most popular theory of pathogenesis of acute appendicitis is the obstruction by fecalith, lymphoid hyperplasia or adhesions of the appendiceal lumen with subsequent secondary infection [4]. However, most of the patients with appendicoliths—composed of firm feces and some mineral deposits—are asymptomatic, but appendicoliths may also cause serious appendicular inflammation and peritonitis.
Diagnosis of appendicitis, particularly in young women, may be challenging. Moreover, in case of abdominal pain in the postoperative period, most physicians would probably first suspect a complication such as bleeding, infection or injury of the bowel or bladder. As it is important to be aware of other causes for the condition, such as acute appendicitis, we herein describe a case of acute appendicitis 3 days after a laparoscopic ovarian cystectomy.
CASE REPORT
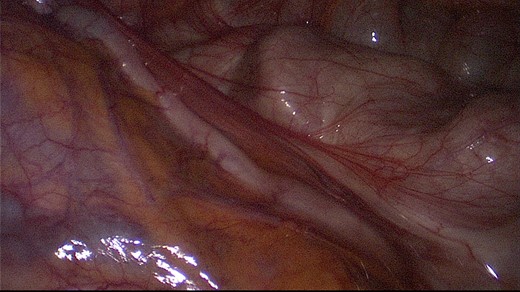
A 26-year-old nulliparous woman presented with right lower and upper abdominal pain 3 days after laparoscopic right ovarian cystectomy (dermoid ovarian cyst) and myomectomy of a small subserous myoma. Intraoperatively, the abdominal organs including the appendix appeared inconspicuous (Fig. 1). She was discharged from the hospital with more abdominal pain than expected, but still in a normal range. The pain increased on her second postoperative day in the evening and the next day, it became severe with concomitant nausea and vomiting.
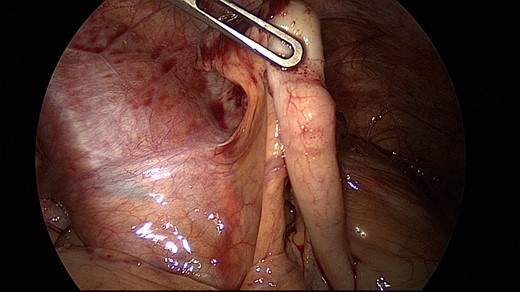
Physical examination revealed normal vital signs, severe diffuse right abdominal tenderness, generalized rebound tenderness, guarding accentuated in the right lower abdomen and rare bowel movements. Laboratory evaluation showed a slightly elevated C-reactive protein (CRP) (17 mg/l, reference <5 mg/l) and an elevated leukocyte count (18 000 cell/mm3, reference <10 200 cell/mm3). Transvaginal and transabdominal ultrasound scanning revealed a normal uterus, a small fluid collection in the Douglas space, an already normal-appearing right ovary, no free fluid in the Morison’s pouch, no pathology of the gallbladder and no lesions suspected to be an abscess. But it showed an increased diameter of the appendix of 8.2 mm, “target sign” on axial scan of the appendix, an appendicolith and periappendiceal fluid of ~2 ml (Fig. 2). Therefore, an immediate re-laparoscopy was indicated, which showed an acute appendicitis and peritonitis (Fig. 3). A laparoscopic appendectomy was performed. The postoperative period was uneventful and the patient was discharged without complication. Pathologic evaluation of the appendix showed an ulcero-phlegmonous, partly abscessing appendicitis, a distal appendicolith of 0.5 cm in diameter and acute peritonitis.
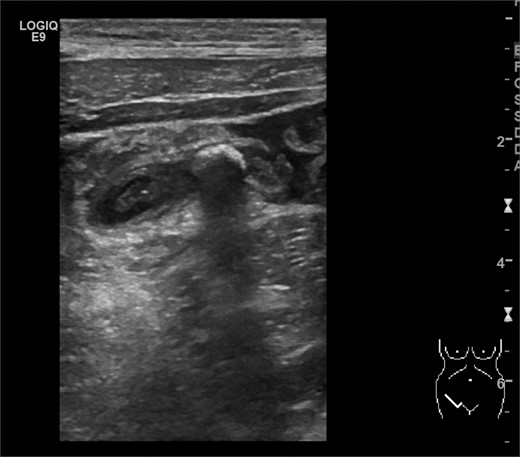
Ultrasonography showing the appendicolith and periappendiceal fluids. (Picture by Markus Buerge, MD)
DISCUSSION
Appendicoliths may be associated with acute appendicitis [5, 6]. Thus, one could consider this case as a coincidence. However, we hypothesize that appendicitis particularly in cases of appendicolithiasis might be triggered by laparoscopic abdominal surgery by influencing yet-unknown factors. Therefore, post-laparoscopic appendicitis might be rather a complication than a coincidence. As we did not find any other case in the literature, there might be very few cases of post-laparoscopic appendicitis or these cases might be underreported. However, one should be aware of appendicitis as a cause of acute postoperative abdominal pain, even if the appendix appeared inconspicuous during the first operation.
Appendicoliths appear to play a role in the pathogenesis of acute appendicitis and are associated with complicated appendicitis [6]. Whether an elective appendectomy in patients with incidentally recognized appendicoliths is indicated or not, is discussed controversially. Some authors recommend considering an elective appendectomy in such cases [6], whereas others conclude that the incidental finding of an appendicolith without signs of appendicitis on imaging studies is no indication for appendectomy [7, 8]. However, if an elective laparoscopy is indicated for another reason, such as ovarian cystectomy, myomectomy or endometriosis, according to certain authors incidental appendectomy may be of benefit in young patients in the prevention of future morbidity and mortality following an acute appendicitis as well as it may reduce disability, time and costs of diagnostic work-up in case of future abdominal pain [9, 10]. Incidental appendectomies in women undergoing gynecological laparoscopy have an extremely low complication rate, require a short amount of time and are cost-effective [10]. However, the extent of long-term complications of this potentially superfluous additional trauma, such as adhesions followed by bowel obstructions and infertility, is unknown. Also, one should keep in mind the potential adverse effects of an appendectomy, such as the possible association between appendectomy and an increased risk for colorectal cancer and Crohn’s disease. Nonetheless, further study about the risk and benefit of incidental appendectomies particularly in young patients with appendicolithiasis undergoing elective abdominal surgery might be of great value as one might reduce morbidity and costs by reintroducing incidental appendectomies in cases of appendicoliths. And one should always consider acute appendicitis as a possible cause of post-laparoscopic abdominal pain.
ACKNOWLEDGMENTS
The authors would like to thank M. Buerge, MD, for the ultrasonographic pictures, and L. Duelli and M. Gallmann, for proofreading.
CONFLICT OF INTEREST STATEMENT
None declared.



