-
PDF
- Split View
-
Views
-
Cite
Cite
Ashwad Afzal, Ivan Wong, Aleksandr Korniyenko, Alex Ivanov, Berhane Worku, Iosif Gulkarov, Superior vena cava syndrome from an invasive thymoma with transcaval invasion to the right atrium, Journal of Surgical Case Reports, Volume 2016, Issue 4, April 2016, rjw044, https://doi.org/10.1093/jscr/rjw044
Close - Share Icon Share
Abstract
Invasive thymoma with transcaval extension to the right atrium is a rare cause of superior vena cava syndrome. We present a case on a 74-year-old female presenting with dyspnea on exertion, and facial and upper extremity swelling. Physical examination revealed mild facial swelling, non-pitting edema involving the upper extremities and distention of superficial veins of the anterior chest wall and jugular veins. An echocardiogram showed moderate right atrial dilation with a mobile mass in the atrial cavity prolapsing through the tricuspid valve. Cardiac magnetic resonance imaging revealed a 9.9 × 4.3 cm heterogeneous mass in the anterior mediastinum compressing the superior vena cava and endovenously extending into the right atrium. Tissue biopsy of the mediastinal mass revealed a type B1 thymoma, further staged as a Masaoka IVa invasive thymoma that underwent successful en bloc resection followed by removal of intracaval and right atrial mass.
INTRODUCTION
Superior vena cava (SVC) syndrome is a rare presentation of invasive thymomas. Presentation can vary significantly based on the extent of tumor invasion and associated paraneoplastic syndromes. We present a case of SVC syndrome from a type B1, Masaoka stage IVa invasive thymoma that was invading multiple mediastinal structures including the superior vena cava, right atrium, pericardium and right upper lung lobe.
CASE REPORT
A 74-year-old female presented with facial and upper extremity swelling over the last month. The swelling was worse in the morning and improved throughout the day. The patent also reported dyspnea on exertion. A review of systems was otherwise negative. Social history was notable for 40-pack-year smoking history, but she quit smoking 12 years ago. Her vital sign were stable. Physical examination revealed mild facial swelling, non-pitting edema of the upper extremities and distention of superficial veins of the anterior chest wall and jugular veins. There were no significant laboratory abnormalities. An echocardiogram showed moderate right atrial dilation with a mobile mass in the atrial cavity prolapsing through the tricuspid valve, bowing of atrial septum from right to left consistent with increased right atrial pressure, moderate tricuspid regurgitation and normal left ventricular ejection fraction with no regional wall motion abnormalities. Cardiovascular magnetic resonance imaging revealed a 9.9 × 4.3 cm heterogeneous mass admixed with thrombus in the anterior mediastinum compressing the SVC and endovenously extending into the right atrium (Figs 1–3). Anticoagulation with heparin drip was initiated. A computed tomography (CT)-guided biopsy revealed a tan-colored mass with CD5 lymphocyte predominance, inconspicuous epithelial cells positive for P63 expression and cytokeratin AE1/AE3 that was morphologically consistent with thymoma type B1.
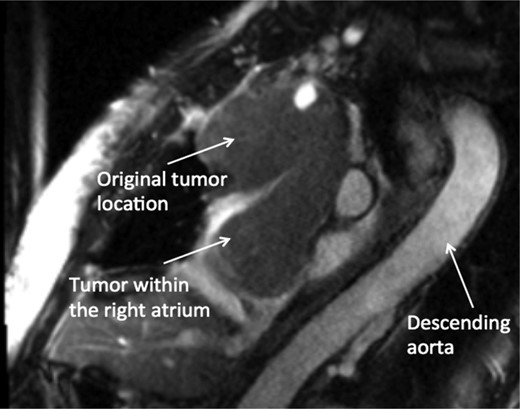
CMR sagittal view: large anterior mediastinal mass with extension into the right atrium.
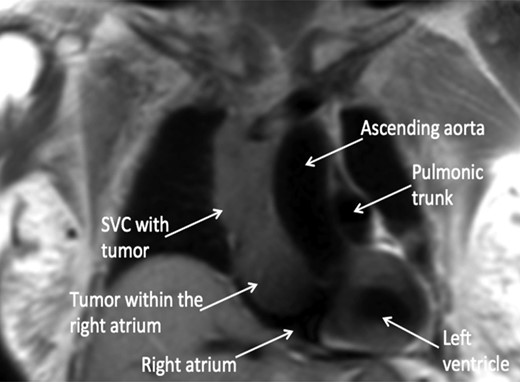
CMR coronal view: anterior mediastinal mass invading superior vena cava and extending into the right atrium.
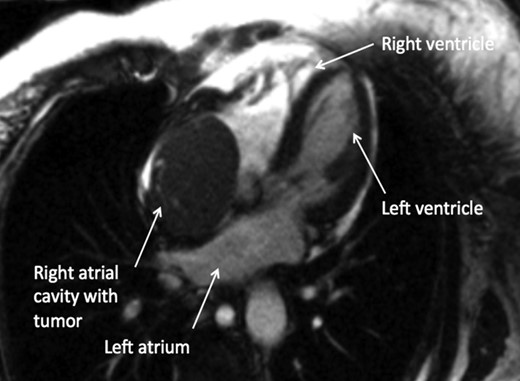
CMR axial four-chamber view: mass in the right atrial cavity protruding through the tricuspid valve into the right ventricle.
An open thymectomy was performed via median sternotomy. A large tan-colored mediastinal mass was found infiltrating the right upper lobe of the lung, pericardium, right phrenic nerve, brachiocephalic vein, right innominate vein, SVC and the right atrium. The mediastinal mass was resected followed by wedge resection of the right upper lobe that was densely adherent to. The right phrenic nerve had to be sacrificed. Cardiopulmonary bypass was then initiated, maintaining a flow of 2.4 l/min and a mean arterial pressure of 70 mmHg. Snares were placed over the SVC, inferior vena cava and innominate vein after cannulation. Once the snare was tightened, the right atrium was then opened followed by removal of a 6.5 × 6.0 × 4.8 cm tan-colored mass with thrombus that was penetrating into the SVC. There was tumor infiltration of the SVC which required excision and reconstruction with a Gortex patch. There was no nodal involvement. Cardiopulmonary bypass was weaned off successfully. The mass was classified as a stage IVa invasive thymoma using the Masaoka classification due to pleural and pericardial invasion. There were no postoperative complications and the swelling of the face and upper extremity improved. No postoperative anticoagulation was required. Patient was further treated with radiation therapy to reduce the risk of recurrence. Patient is being followed in the outpatient radiation oncology clinic and is recurrence free at 3 years.
DISCUSSION
Thymoma is a rare neoplasm primarily arising within the anterior mediastinum. Invasive thymoma commonly invades surrounding thoracic structures such as the heart, lungs and vessels causing compressive symptoms. Most thymomas with cardiac involvement are limited to the pericardium and very few cases of transcaval extension with intracardiac involvement have been reported [1, 2]. SVC syndrome typically arises from extrinsic compression and less commonly from transcaval thymoma infiltration [3]. Initial diagnostic evaluation of thymomas involves investigation of paraneoplastic syndromes of which myasthenia gravis is the most common [4–6]. Imaging test involves a CT scan or an MRI to evaluate the mass and its surrounding structure for potential resection. A definitive diagnosis requires biopsy and treatment is based on histologic classification and staging. Our case is a type B1 thymoma characterized by CD5 lymphocyte predominance, inconspicuous epithelial cells positive for P63 expression and cytokeratin AE1/AE3 using the World Health Organization histologic classification [7]. The Masaoka classification was stage IVa as there were pleural and pericardial invasion with no evidence of lymph node involvement or distant hematogenous spread [8]. Both histologic characteristics and tumor staging are independent prognostic factors [5, 9]. The invasiveness of a type B1 thymoma is 73.3% and the potential to invade greater vessels is 6.6% [5]. A retrospective study by Rena et al. showed a 10-year disease-free survival of 85% with a 5-year relapse rate between 2 and 10% for type B1 thymoma after complete resection followed by either radiation therapy, chemotherapy or a combination of both. There were no stage IVa thymomas that reached a 10-year follow-up, but disease-free survival after 5 years was 61% [5]. However, a larger study by Ströbel et al. [10] showed a 10-year survival probability of 47% for stage IV tumors.
This case highlights SVC syndrome from an invasive type B1, Masaoka stage IVa thymoma causing extrinsic compression with transcaval infiltration to the right atrium. Successful resection under cardiopulmonary bypass can be performed and further treatment with radiation therapy reduces the risk of recurrence.
CONFLICT OF INTEREST STATEMENT
The authors have declared no conflicts of interest. This manuscript has not been submitted for publication; it has not been accepted for publication and has not been published in any other journal. All authors have read and approved the final version of the manuscript.
REFERENCES
- echocardiography
- edema
- superior vena cava syndrome
- right atrium
- tricuspid valve
- atrium
- biopsy
- superior vena cava
- physical examination
- heterogeneity
- dilatation, pathologic
- face
- jugular veins
- thymoma
- arm
- cardiac mri
- exertional dyspnea
- superficial veins
- mediastinal mass
- right atrial mass
- anterior chest wall
- anterior mediastinum
- facial swelling



