-
PDF
- Split View
-
Views
-
Cite
Cite
Satnam Singh Rehal, Mustansir Alibhai, Esther Perera, Post-traumatic Lipoma of the Parotid gland, Journal of Surgical Case Reports, Volume 2016, Issue 4, April 2016, rjw041, https://doi.org/10.1093/jscr/rjw041
Close - Share Icon Share
Abstract
Lipoma of the parotid gland is a rare entity. Trauma with soft tissue haematoma formation and subsequent lymphatic effusion, fat necrosis and lipoma formation have been postulated as an aetiological pathway. We report a case of a post-traumatic lipoma of the parotid gland to add to the available literature on this uncommon pathology.
INTRODUCTION
Lipoma is a thinly encapsulated benign tumour of mesenchymal origin and is found within parts of the body where fat is normally present. Accounting for 0.1–5% of all benign tumours, lipomas may occur either as single or multiple entities [1]. Less than 15% of all cases occur in the head and neck region. Here, lipomas tend to arise mainly in the posterior cervical triangle and forehead, commonly in the fourth to sixth decades of life. On rarer occasions, lipomas may occur in the pharynx, larynx, oral cavity, parotid and submandibular areas [1, 2]. Comprising 0.6–4.4% of all parotid tumours, a lipoma of the parotid gland is a rare entity [3]. They most frequently present as a painless slowly enlarging mass. Preoperative evaluation techniques including the use of ultrasound (US), fine needle aspiration cytology (FNAC), magnetic resonance imaging (MRI) and computed tomography (CT) have enabled a more accurate assessment of these tumours and a rational approach to their management. The aetiology remains largely idiopathic, but literature suggests a plausible genetic predisposition [2, 4]. There is increasing evidence for trauma-induced haematomas and subsequent lipoma formation [5]. Histologically, lipomas contain fat cells although morphological variants containing other mesenchymal tissues can be present such as angiolipoma and osteolipoma. We present a rare case of a post-traumatic lipoma of the parotid gland, describing the diagnostic workup and surgical removal.
CASE REPORT
A 53-year-old female initially presented to the emergency department following an assault in which she sustained a punch to the left side of her jaw. Her medical history of note was type 2 diabetes, hypertension and hypercholesterolaemia. Clinical and radiographical examination revealed a left high condylar head fracture (Fig. 1). Her occlusion was stable and non-surgical management was employed. On 2-month review, she complained of a persistent, painless, slow growing mass in the left pre-auricular area. Clinical examination revealed a soft, mobile, non-tender, non-fluctuant, regular mass within the left parotid gland with normal overlying skin and normal sensation. There was no associated cervical lymphadenopathy and facial nerve function was intact.

Orthopantomographic image showing a left high condylar head fracture and a stable occlusion with adequate posterior contact.
An US scan showed a well-defined non-vascular hypoechoic lesion in the left superficial parotid lobe measuring 3.2 × 2.2 × 2.6 cm (Fig. 2). The corresponding fine needle aspirate cytology was inconclusive. MRI showed high signal intensity on T1-weighted images (Fig. 3) and a branching vessel-like central structure traversing the lesion. These results were consistent with a lipomatous lesion. Surgical removal was performed via an extra-capsular dissection with facial nerve preservation. The tumour comprised of a well-circumscribed, soft yellow, fatty mass covered in a thin fibrous capsule (Fig. 4). Postoperative facial nerve function was normal with transient altered sensation to the ear lobe. Histopathology showed a homogenous proliferation of mature adipocytes, confirming the diagnosis of a lipoma. On 6-month review, there are no signs of recurrence.
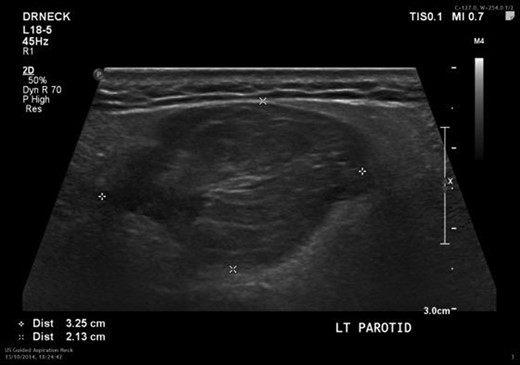
Ultrasound of the left parotid gland showing a well-circumscribed hypoechoic lesion.

Coronal MRI showing the extent of the lipoma and vessel-like structure traversing it (arrow).

The resected parotid lipoma enclosed within a thin fibrous capsule.
DISCUSSION
Adipose tissue is normally present in the parotid gland; however, the incidence of lipomas here is very low [3]. The presence of a fibrous capsule helps to distinguish them from simple fat aggregations. Different causes of lipomas are mentioned in the literature: heredity, obesity, diabetes, radiation, endocrine disorders, insulin injection, corticosteroid therapy and trauma [6]. As in this case, a preceding trauma to the soft tissues has been hypothesized to result in a haematoma, with subsequent lymphatic effusion, fat necrosis and lipoma formation [5]. As for their rarity in the parotid gland, lipomas are seldom considered in the preoperative differential diagnosis. The principle consideration of an intraparotid mass is to differentiate between benign and malignant salivary gland neoplasia. There is, however, no unique clinical feature by which the lipoma can be separated from other parotid gland tumours.
With a sex ratio of 5 : 1, parotid lipomas occur more frequently in males than females [5–7]. The majority of patients present with a single lesion usually without any predisposing causal factors [7]. They progress slowly as soft well-delineated asymptomatic masses where the main patient concern is of the associated cosmetic asymmetry. On average, 75% of the lesions are located within the superficial lobe with a further 6.5% in the deep lobe, and 16.5% occurring in both the deep and superficial lobes [7]. Clinical diagnosis alone is difficult and therefore medical imaging is essential. As is standard in the workup of parotid masses, US and FNAC provide combined imaging and cytological diagnosis although in lipoma the cytology is often inconclusive [8]. An MRI scan is the imaging modality of choice for further assessment prior to any planned surgical excision. It will identify soft tissue margin characteristics and accurately help differentiate between benign and malignant lesions.
The surgical approach to a parotid lipoma excision should be the same as for any other suspected benign tumour, with due regard to the presence of the facial nerve in the operative field. It is unusual for the facial nerve to be involved preoperatively; however, a single case with complete palsy has been reported in the literature [9]. During surgery, the facial nerve is identified and followed up to its peripheral branches as far as necessary for complete tumour dissection. As in this case, the use of facial nerve monitoring helps in protecting nerve function. Recurrence after adequate resection is very rare [10].
Surgeons and physicians alike should be aware of the possibility of lipomas presenting within the parotid gland, and should recognize its formation in the post-trauma situation and its inclusion in the differential diagnosis of parotid lesions. Surgeons should be familiar with its management which is in keeping with the overall workup of any parotid mass.
CONFLICT OF INTEREST STATEMENT
None declared.
ACKNOWLEDGEMENTS
We thank the patient for consenting to the reporting of her uncommon sequel of events.



