-
PDF
- Split View
-
Views
-
Cite
Cite
Vadim Meytes, Steven P. Schulberg, Nicholas Morin, Galina Glinik, Undiagnosed hypothyroidism presenting with sigmoid volvulus, Journal of Surgical Case Reports, Volume 2016, Issue 4, April 2016, rjw033, https://doi.org/10.1093/jscr/rjw033
Close - Share Icon Share
Abstract
The incidence of hypothyroidism presenting with sigmoid volvulus, a phenomenon known as myxedema pseudovolvulus, is exceedingly rare. A male in his late thirties presented to our institution with a chief complaint of abdominal pain. The patient underwent CT scan, which was consistent with massive colonic dilatation with sigmoid volvulus. He was taken to the operating room for exploration and was found to have sigmoid volvulus and underwent a segmental resection. Postoperatively, the patient was newly diagnosed with severe hypothyroidism.
INTRODUCTION
Colonic volvulus ranks as the third most common cause of large-bowel obstruction in the USA following cancer and diverticulitis. It is estimated that volvulus is responsible for ∼5% of all cases of intestinal obstructions and 10–15% of large-bowel obstructions. The sigmoid colon (80%) is the most common site of large-bowel torsion followed by the cecum (15%), transverse colon (3%), and the splenic flexure (2%) [1]. Additionally, hypothyroidism is extremely prevalent in the US population, affecting an estimated 4.6% of the general population [2]. These two diseases can present together. Severe hypothyroidism presenting with colonic dilation is known as myxedema pseudovolvulus. It is exceedingly rare and has only been described in small case series in literature [3–6]. Here, we present such a case.
CASE REPORT
A male in his late thirties presented to our institution with a chief complaint of abdominal pain. The patient reported 3 days of worsening, generalized abdominal pain with constipation that had progressed to obstipation. The patient also admitted to increased lethargy over the past 6 months. He denied nausea, vomiting, depressed mood and any other psychiatric or neurologic complaints. Past medical history was significant for gastrointestinal reflux and chronic constipation. The patient denied taking any medications regularly, and his social and family histories were non-contributory.
On presentation, the patient had blood work drawn with the following results: WBC count was 5.1k/μl, hemoglobin 9.6 g/dl, hematocrit 28.2%, platelet count 167k/μl, total bilirubin 1.0 mg/dl, direct bilirubin 0.3 mg/dl, AST 95 IU/l, ALT 87 IU/l, alkaline phosphatase 64 IU/l, GGT 28 IU/l, LDH 377 IU/l, amylase 55 U/l, lipase 27 U/l and lactate 2.0 mmol/l.
The patient's chest X-ray showed gaseous distention of the colon prompting further investigation. He was then sent for CT scan of his abdomen, revealing distention of the colon with swirling of mesentery in the left lower abdomen, and superior displacement of the sigmoid colon consistent with sigmoid volvulus (Fig. 1).
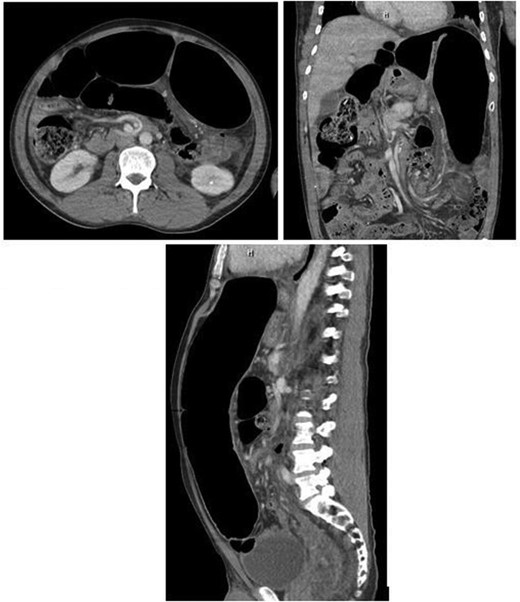
CT scan findings showing significant sigmoid colonic dilatation with concerns for sigmoid volvulus.
The patient was then taken emergently to the operating room for decompression and exploration. Intraoperatively, there was a finding of a large dilated sigmoid colon with point of torsion at a dense adhesion of the colon with small bowel mesentery. The colonic diameter was >10 cm with collapse of the proximal and distal segments. Colonic ischaemia was present prior to untwisting the volvulus. Following detorsion, warm soaked laparotomy pads were applied to the affected sigmoid colon; however, there were no signs of reperfusion. As a result, the patient then underwent a sigmoid resection with primary anastomosis of the descending colon and the rectum. The resected specimen can be seen in Fig. 2. No other intraoperative abnormalities were found. Post-operatively, the patient's diet was slowly advanced with the return of normal bowel function on the third postoperative day. As part of an evaluation to the cause of the patient's chronic constipation, a thyroid panel was sent with the following results: TSH >150 mc/ml, Free T3: <0.2 pg/ml, Free T4: 0.12 ng/dl.

The patient was newly diagnosed with hypothyroidism and was started on thyroid hormone replacement therapy using levothyroxine sodium. The patient had an uncomplicated hospital course during which lethargy improved. The patient was sent home tolerating a regular diet, having regular bowel movements, and was prescribed continuing thyroid hormone replacement. The final histopathology on the surgically resected specimen revealed benign colonic mucosa with edema and lymphoid aggregates along with diverticulosis coli.
DISCUSSION
Hypothyroidism is an extremely common diagnosis in the US population. It can present with a number of nonspecific symptoms which, when taken as a whole, can help reveal the diagnosis. Among those common complaints are constipation and vague abdominal pain. If hypothyroidism progresses without diagnosis, colonic manifestations, such as pseudo-obstruction secondary to hypothyroid myxedema, can be the presenting diagnosis. Though this phenomenon is exceedingly rare, with only a small number of case reports describing its prevalence, admitting physicians should consider hypothyroid myxedema in patients presenting with megacolon and colonic pseudo-obstruction.
The pathology and pathophysiology in this and similar cases are unique to the disorder. The megacolon caused by decreased peristalsis and increased edema secondary to deposition of hydrophilic glycoproteins in the colonic wall [3]. It has been described in prior cases that on gross examination, a thickened colon with lost elasticity was identified. On further microscopic examination of these specimens, myxedematous and lymphocytic infiltration of the stroma and submucosa was noted. This infiltrate, coupled with the loss of elasticity, is thought to mechanically alter impulse transmission at the myoneural junctions of the colon leading to ileus and eventual megacolon [3–5].
If identified early, thyroid replacement therapy usually leads to resolution of the patient's colonic symptoms [4–6]. Once hypothyroidism is the presumed cause of abdominal symptoms, these patients should be tested and hormone replacement therapy should be started immediately. However, if the patient's symptoms are not recognized early, they can progress to true sigmoid volvulus. Once volvulus occurs, it can quickly become a surgical emergency requiring acute intervention, as was the case with our patient.
A clinician examining a patient presenting similarly to ours should always have hypothyroidism in their mind as a possible underlying etiology of the pseudo-obstruction. If there is a high clinical suspicion for hypothyroidism based on other symptoms reported by the patient, a thyroid stimulating hormone level should be ordered. If hypothyroidism is confirmed, the patient can be started on hormone replacement and closely followed to ideally prevent a trip to the operating room. However, if clinically the patient deteriorates, the patient should be urgently taken to surgery. This raises the question of routine thyroid testing in patients with colonic distension that could lead to volvulus. Though myxedema pseudovolvulus is rare, TSH screening is cheap and efficient in ruling out an etiology that can be treated nonsurgically. The main determinant for testing in these cases should be the presence of other symptoms in the hypothyroid constellation such as chronic fatigue, depression, or hair loss.
Myxedema pseudovolvulus is a rare late complication of undiagnosed hypothyroidism. Patients can present with sigmoid volvulus, a surgical emergency. It should be suspected as a possible differential diagnosis in patients presenting with years of chronic constipation, lethargy, and possible prior history of megacolon or pseudo-obstruction. The patient's clinical picture guides surgical management; however, all of these patients should be started on hormone replacement therapy after being diagnosed with hypothyroidism. We believe that prompt diagnosis and a high level of suspicion can lead to successful nonoperative treatment of patients who present with colonic dilation secondary to hypothyroidism.
CONFLICT OF INTEREST STATEMENT
None declared.



