-
PDF
- Split View
-
Views
-
Cite
Cite
Mangaladevi S. Patil, Kristopher M. Day, Bassam I. Aswad, Jesse Hart, Thomas Ng, A case of recurrent desmoplastic malignant melanoma presenting as empyema with underlying lung mass, Journal of Surgical Case Reports, Volume 2016, Issue 4, April 2016, rjw029, https://doi.org/10.1093/jscr/rjw029
Close - Share Icon Share
Abstract
Desmoplastic malignant melanoma (DMM) is an extremely rare subtype of cutaneous melanoma that has diverse clinical presentations. We describe the unique case of a 57-year-old man presenting with empyema secondary to vascular occlusion from metastatic DMM. Only two other cases of DMM presenting as a lung mass have been previously reported in the literature. This report highlights potential insidious pathology of DMM, which requires a high clinical suspicion to properly diagnose and manage.
INTRODUCTION
Malignant melanoma is known for its highly unpredictable natural history and a wide array of presentations. Desmoplastic malignant melanoma (DMM) is a rare form of malignant melanoma characterized by spindled malignant melanocytes within a fibrocollagenous stroma and may demonstrate neurotropic features. This uncommon variant accounts for <5% of all cutaneous melanoma and was first described by Conley et al. in 1971 [1]. It commonly presents in older males on sun-exposed areas such as the head and neck [2, 3]. Five-year survival trends are comparable with similar stage non-desmoplastic malignant melanoma (NDMM). Later stage presentation may be more common due to a high frequency of amelanotic lesions in DMM.
CASE REPORT
A 57-year-old male with a past medical history of stage IIB (T3b, N0) melanoma of the right superior neck and heavy marijuana use presented to the emergency department in April 2015 with progressively worsening dyspnea, right-sided pleuritic pain and hemoptysis. The patient was afebrile and normotensive. Physical examination was unremarkable except for decreased breath sounds at the right lung base. Laboratory values were within normal range and showed no leukocytosis. A subsequent chest X-ray showed right-sided hydropneumothorax with mild right-to-left mediastinal shift (Fig. 1A). A chest computed tomography (CT) scan confirmed the presence of a right infrahilar mass (Fig. 1B). The patient was admitted to the medicine service for management of hydropneumothorax.
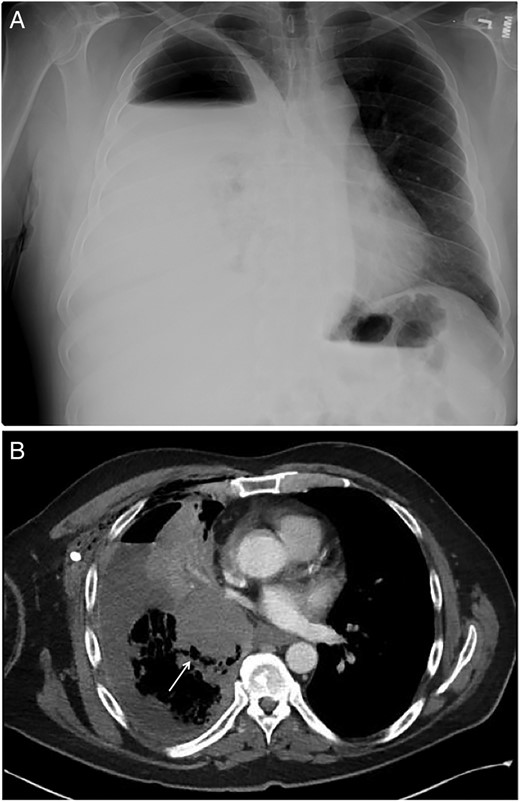
(A) Anterior–posterior chest X-ray showing large right-sided hydropneumothorax with mild right-to-left mediastinal shift. (B) Chest CT showing a right infrahilar mass (arrow) occluding bronchus intermedius with post-obstructive airspace disease within the right lower lobe.
A 14-French image-guided pigtail catheter was placed into right-sided pleural effusion draining over 2 l of purulent fluid which was sent for cytology, aerobic and anaerobic culture, and cell count. Cytology was negative for malignancy, and culture revealed Streptococcus viridians. A second CT-guided chest tube was placed 3 days later due to persistent hydropneumothorax with further drainage of 200 ml of purulent fluid. Subsequent catheter-directed TPA therapy initially demonstrated improvement in the effusion, but a post-procedural chest X-ray demonstrated a non-expanded lung, consistent with trapped lung.
Bronchoscopy and endobronchial ultrasound with biopsy were then performed. Bronchoscopy revealed occlusion of the bronchus intermedius by extrinsic compression rather than from an endoluminal tumor. The bronchus intermedius was biopsied showing bronchial tissue with mild subepithelial chronic inflammation without evidence of malignancy.
The patient was then consulted for surgical diagnostic and management options. The initial operative plan was decortication to re-expand the trapped lung. Intra-operatively, however, a necrosis was unexpectedly found in the lower and middle lobes and resected; on gross examination, the lower and middle pulmonary arteries and veins were thrombosed by intraluminal tumor. In addition to lobectomy, rib resection for open flap drainage was performed due to the presence of a large residual empyema space. Pathology revealed metastatic melanoma with intravenous tumor (Fig. 2A) positive for S100 protein (Fig. 2B) and SOX10 (Fig. 2C); HMB45 and MelanA were negative. Microscopic comparison with the previous melanoma excised from the patient's neck in 2012 was consistent with lung metastasis from that tumor.
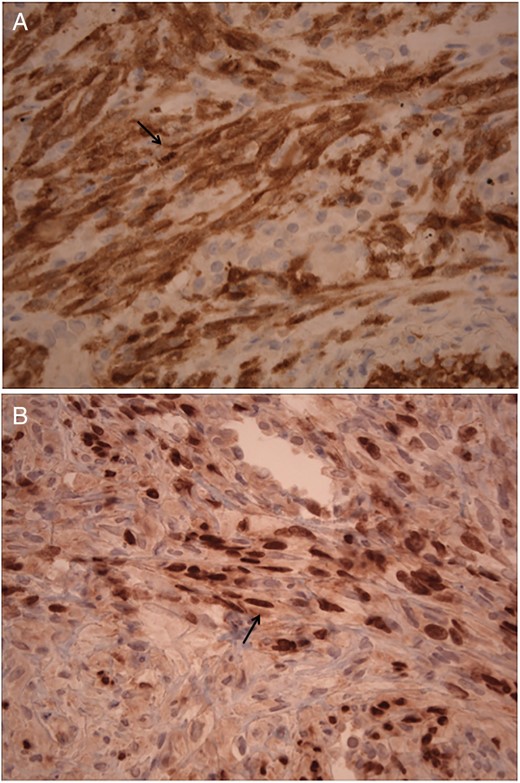
(A) 400× Histology of infiltrating melanocytes and diffuse desmoplasia within lung parenchyma and immunohistochemistry showing tumor cells staining positive for S100 (arrow). (B) 400× Histology demonstrating periarteriolar involvement, spindle cell formation and immunohistochemistry showing tumor cells stain positive with and nuclear SOX10 (arrow).
The patient experienced resolution of the empyema with drainage and removal of the associated necrotic neoplastic lung tissue. He is alive and currently being restaged by oncology and considered for nivolumab treatment.
DISCUSSION
We present a case that is consistent with the usual clinical presentation of DMM: a middle-aged male with a primary tumor in the head and neck region. However, our patient's recurrent cancer uniquely manifested as a lung mass complicated by an empyema secondary to right middle and lower lobe necrosis due to occlusive tumor vascular infiltration. DMM is known to disseminate hematogenously but very rarely presents as a lung mass, which has only been reported twice in the literature, neither of which were associated with an empyema [4, 5].
In contrast to NDMM, which may spread to distant sites, DMM exhibits a more sarcomatoid local recurrence pattern. Regional lymph node involvement is detected up to 13.7% of the time in pure and mixed DMM [6]. Strong and diffuse S100 and SOX10 immunohistochemical staining was observed in this case, which is necessary to confirm the diagnosis, since conventional melanocyte-specific markers (Melan A and HMB45) are characteristically negative in DMM (4, Fig. 2).
The role of both radiation and immunotherapy or chemotherapy is under investigation, as DMM's hybrid morphology and recurrence pattern suggest that it may respond to treatment similarly to sarcoma or NDMM [2, 7]. There are currently no standardized treatment strategies other than complete surgical resection with adequate margins, which achieves 5-year survival in 61% of patients [5].
The long-term clinical course of DMM is variable and typically results in local recurrence, though distant metastases occur in ∼15% of patients [2]. Our patient's original tumor was 2.1 mm thick. Previous studies in NDMM suggest that greater depth of invasion correlates with the development of systemic metastases [2]. We observed a disease-free interval of nearly 3 years prior to detection of the lung mass. This case illustrates a unique presentation of recurrent DMM with lung mass and empyema years after primary tumor resection, reminding clinicians to maintain a high index of suspicion for atypical modes of recurrent tumor presentation in DMM patients.
CONFLICT OF INTEREST STATEMENT
None declared.



