-
PDF
- Split View
-
Views
-
Cite
Cite
Vishal Bhalla, Nadir Khan, Matthew Isles, Pott's puffy tumour: the usefulness of MRI in complicated sinusitis, Journal of Surgical Case Reports, Volume 2016, Issue 3, March 2016, rjw038, https://doi.org/10.1093/jscr/rjw038
Close - Share Icon Share
Abstract
The sinuses are common sites of infection in children, and if clinical presentation is delayed, there is a high risk of complications including intracranial spread. We present a case of a 5-year-old boy who presented with non-specific symptoms of sinusitis. He went on to develop osteomyelitis of the frontal bone and a subperiosteal abscess known as Pott's puffy tumour. Whilst computed tomography provides an excellent initial imaging, this case report emphasizes the advantages of magnetic resonance imaging, especially when there is extensive involvement of the sinuses with an absence of ionizing radiation. Prompt surgical treatment is imperative as there is a potential for significant morbidity if not quickly diagnosed and treated.
INTRODUCTION
Pott's puffy tumour was first described by Sir Percival Pott in 1775 as a frontal swelling with an associated subperiosteal abscess and an extradural empyema [1]. This condition has become rarer with the advent of modern antibiotic therapy; however, in paediatric patients, the diagnosis can be delayed as presenting symptoms and signs can be non-specific by which time intracranial complications may develop.
CASE REPORT
We present a case of a 5-year-old boy who presented with a 2-week history of fluctuating headache and fever with nasal congestion and a decreased energy level. The patient was initially treated with oral antibiotic therapy; however, he attended the Children's Assessment Unit in Accident and Emergency after developing a 2-day history of a painful swelling over the forehead with overlying redness.
On clinical examination, swelling and overlying redness were noted over the right aspect of the forehead and in particular the patient complained of tenderness on upward gaze; however, the remainder of the neurological examination was unremarkable at the time.
An initial computed tomography (CT) head with contrast (Fig. 1) revealed completely occluded sphenoid, ethmoid, frontal and maxillary sinuses. There was a rim enhancing area of low attenuation over the frontal bone in keeping with a subperiosteal collection, although no bony erosions were apparent. No intracranial spread was seen, although there was a small subperiosteal collection in the right orbit medial to the right medial rectus muscle.
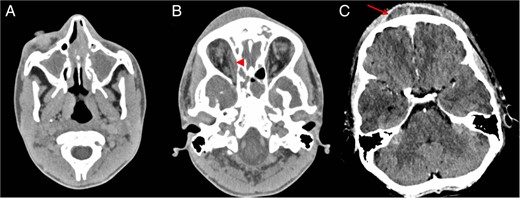
Post-contrast axial CT (A) shows opacified paranasal sinuses keeping with sinusitis. Right orbital subperiosteal abscess (arrowhead) and scalp subperiosteal abscess (arrow) consistent with Pott's puffy tumour seen on CT (B and C).
The patient was immediately referred to the ENT team and underwent a right functional endoscopic sinus surgery plus medial orbital decompression for a right-sided periorbital cellulitis/collection. At endoscopy, he was also noted to have Grade 1 nasal polyps and mucosal thickening, in keeping with underlying sinusitis in the maxillary antrum and ethmoids. His intra-orbital compression was relieved by endoscopic removal of the lamina papyracea, leaving the orbital periosteum intact.
Two days following this procedure, the patient had persistent tenderness over the forehead. At this point, we decided to proceed to magnetic resonance imaging (MRI) (Fig. 2) to further evaluate the frontal bone and extra-axial spaces. These images confirmed abnormal signal within the frontal bone in keeping with osteomyelitis. Post-contrast-enhanced images demonstrated scalp and intra-dural enhancement. Diffusion-weighted images confirmed an evolving epidural abscess that was encroaching and slightly compressing the superior sagittal sinus, although the sinus remained patent with no evidence of thrombosis.
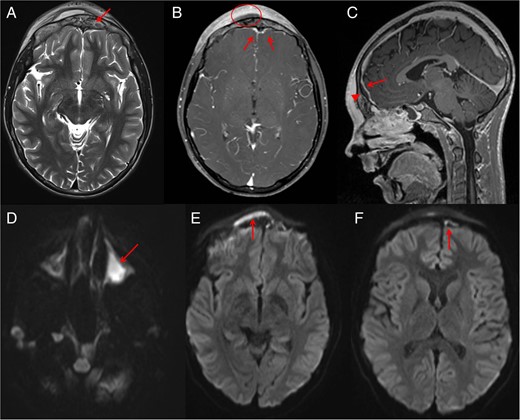
Post-drainage of right maxillary sinus and right orbital subperiosteal abscess MRI was performed. MRI shows abnormal signals (arrow) from the anterior frontal bone suggesting osteomyelitis (A). Post-contrast MRI demonstrates the scalp Pott's puffy tumour (circle) with surrounding scalp enhancement. MRI (B) also shows reactive dural enhancement and an epidural abscess that is better seen (arrowhead) on sagittal sequence (C) compressing the superior sagittal sinus (arrow) which is not thrombosed. Diffusion images (D–F) confirm pus in left maxillary sinus (D), scalp subperiosteal abscess (E) and intracranial extra-axial (F) epidural abscess (arrows).
The patient was subsequently referred to the paediatric neurosurgical unit in view of the intracranial infection, although it was decided to proceed with conservative treatment with i.v. antibiotics including Clindamycin, Ceftriaxone and Metronidazole with frontal sinus irrigation. The patient was discharged with 6 weeks of oral antibiotics, and a consequent study taken 2 months following initial admission showed complete resolution.
DISCUSSION
Pott's puffy tumour was first described in 1770 by Sir Percival Pott as a soft ‘doughy’ tumour of the scalp. These features are now known to be a sequel of frontal bone osteomyelitis with an associated subperiosteal abscess. The abscess is often well circumscribed and convex in appearance due to the tight adherence between the periosteum and the frontal bone [2]. Frontal sinusitis remains the single most common cause of Pott's puffy tumour and most commonly second to haematogenous spread of infection, although direct spread post-trauma has also been described [3].
In paediatric patients, clinical symptoms can often be non-specific and vary depending on the severity of infection; a rather indolent course may consist of headache, rhinorrhoea and fever. There should be a high index of suspicion for Pott's puffy tumour when patients develop a fluctuant, tender swelling of the scalp. CT is an excellent initial imaging modality as it is fast, readily accessible and shows good bony detail. If there are any neurological signs such as those of raised intracranial pressure, nausea, vomiting or a focal neurological deficit, there should be a low threshold for MRI and should include post-contrast and diffusion-weighted images. In our case, even with the absence of initial neurological signs, MRI was still performed as it helps to determine the full extent of intracranial involvement that may not be initially evident [4] (Fig. 2).
The diagnosis of Pott's puffy tumour is a surgical emergency. With modern surgical advances, this condition can be treated with minimally invasive techniques such as functional endoscopic sinus surgery, which is particularly useful in paediatric patients. In cases of intracranial extension, there is often a multidisciplinary approach to therapeutics with ENT and neurosurgical specialities involved in treatment. Diseased bone often warrants removal as it may act as a lead point to further repeated infections or may develop necrosis. Small extradural collections are often treated conservatively with i.v. antibiotics; however, aspiration and biopsy have been implemented in order to culture less common organisms responsible for more aggressive infections.
Pott's puffy tumour is a severe complication of frontal sinusitis. A low threshold for imaging should be used to when there is a high index of suspicion. CT is an excellent form of initial imaging to initiate rapid treatment, although MRI is a powerful imaging tool as it can assess the extent of infection, osteomyelitis and intracranial spread. MRI also avoids ionizing radiation, which is useful when repeated scans may be necessary to assess response to the treatment. In paediatric patients, in particular, prompt treatment is critical in achieving an optimal outcome.
CONFLICT OF INTEREST STATEMENT
None declared.



