-
PDF
- Split View
-
Views
-
Cite
Cite
Yan Li Goh, Alexander Haworth, Jeremy Wilson, Conor J. Magee, Life-threatening Petersen's hernia following open Beger's procedure, Journal of Surgical Case Reports, Volume 2016, Issue 3, March 2016, rjw036, https://doi.org/10.1093/jscr/rjw036
Close - Share Icon Share
Abstract
Petersen's hernia (an internal hernia between the transverse mesocolon and Roux limb following Roux-en-Y reconstruction) is well described following laparoscopic gastric bypass surgery. We describe a Petersen-type hernia in a patient who had undergone complex open upper gastrointestinal surgery for chronic pancreatitis.
INTRODUCTION
Petersen's hernia is a rare complication of open surgery and has not been previously described following Beger's procedure for chronic pancreatitis.
CASE REPORT
A 72-year-old male presented as an emergency with sudden onset of central and lower abdominal pain, nausea and vomiting. He had a past surgical history of open Beger's procedure (duodenum preserving resection of the pancreatic head) performed 5 years ago for chronic pancreatitis. There were no other significant co-morbidities.
Computed tomography (Fig. 1) demonstrated a closed loop small bowel obstruction involving almost all of the jejunal loops with mesenteric venous congestion suggesting impending ischaemia. The transition point was posterior to the Roux loop.
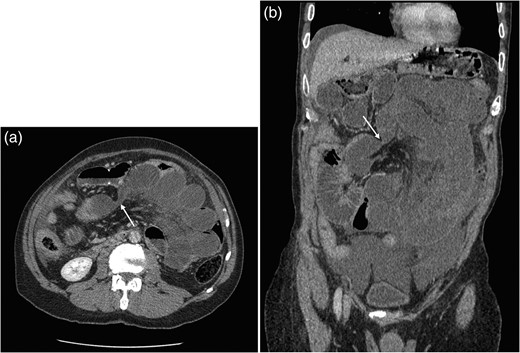
(a and b) Axial and coronal CT images showing obstruction of small bowel with transition point within Petersen's space (arrow).
He underwent emergency laparotomy. At surgery, a type C Petersen's hernia containing 245 cm of infarcted small bowel was encountered. This was resected and a double-barrelled jejuno-ileostomy was fashioned.
The patient was admitted to the intensive care unit for 48 h before being stepped down to a surgical ward. The patient was commenced on total parenteral nutrition in view of his proximal jejunostomy.
The patient had a prolonged in-patient stay of 11 weeks with a high-output stoma but did not require a return to theatre. He was discharged with home parenteral nutrition.
Two months later, he underwent uncomplicated reversal of double-barrelled jejuno-ileostomy and his parenteral nutrition was stopped. His recovery was uneventful and he was discharged 3 days later.
DISCUSSION
Petersen's hernia was first described in 1900 by Dr Petersen where an efferent loop of bowel herniates posterior to the gastrojejunal anastomosis through a space bounded by transverse mesocolon and Roux limb mesentery [1]. Petersen's hernia is an increasingly recognized complication of laparoscopic Roux-en-Y gastric bypass for morbid obesity. It is thought to arise because of a lack of internal adhesions after laparoscopic surgery combined with the significant loss of fat from the small bowel and colonic mesenteries. Three types of Petersen's hernia have been described: Type A involves the alimentary (Roux) limb, Type B involves the bilio-pancreatic limb and Type C involves the common channel [2]. PH can present non-specifically and progress rapidly to bowel infarction, peritonitis and death. Imaging can be inconclusive and clinical awareness with early intervention is important [3].
We are unaware of reports describing Petersen's hernia after Beger's procedure. Beger's procedure is a duodenum preserving resection of the pancreatic head. It is used in refractory chronic pancreatitis when medical therapy fails or when there is a suspicion of malignancy [4]. It involves resection of the pancreatic head whilst preserving the duodenum with a Roux-en-Y reconstruction between the pancreas and jejunum [5].
Petersen's hernia can occur in both laparoscopic and open surgery involving Roux-en-Y reconstruction. It can present as an emergency with bowel obstruction. Clinicians should have a high index of suspicion when assessing patients with previous operations involving Roux-en-Y reconstruction.
CONFLICT OF INTEREST STATEMENT
None declared.



