-
PDF
- Split View
-
Views
-
Cite
Cite
Vinesh Godhania, Lumbar spine osteomyelitis and epidural abscess formation secondary to acupuncture, Journal of Surgical Case Reports, Volume 2016, Issue 3, March 2016, rjw035, https://doi.org/10.1093/jscr/rjw035
Close - Share Icon Share
Abstract
A 39-year-old male with no previous medical history presented with abdominal and low back pain. Based on clinical and radiological findings he was diagnosed with L1/L2 osteomyelitis and epidural abscess. Further history taking revealed recent use of acupuncture for treatment of mechanical back pain. The patient was treated conservatively with an extended course of antibiotics, monitored with repeat MRI scans and had a full recovery with no neurological deficit. This is the first reported case of epidural abscess formation and osteomyelitis after acupuncture in the UK. As acupuncture becomes more commonly used in western countries, it is important to be aware of this rare but serious complication.
INTRODUCTION
Acupuncture is being more commonly used and prescribed in the UK. It is a form of alternative medicine and comes from traditional Chinese medicine. It is used in treating a wide variety of conditions such as musculoskeletal pain and headaches. It is seen as a low-risk complementary therapy that is being administered by many different health professionals. However, alternative medicine is rarely taught in medical school, so doctors may be unaware of the potential risks. This case highlights a rare complication of epidural abscess formation following acupuncture.
CASE REPORT
A 39-year-old man presented to the emergency department with a 1-week history of abdominal pain and 3-week history of back pain. No previous medical or surgical history. On examination the abdomen was soft with mild central tenderness. The back had mild paraspinal tenderness in the lumbar region but no neurology. He was apyrexial. Observations were normal and on admission the white cell count was 8.2 × 109/l and the CRP was 244 mg/l. The patient was referred to general surgeons due to the abdominal pain.
The initial chest and abdominal radiographs were normal but blood tests showed a raised CRP of 244, so broad spectrum antibiotics were started. It was decided that due to the abdominal pain and raised inflammatory markers the patient required a CT abdomen/pelvis which showed para-aortic lymph nodes but no other abnormalities. Testicular lymphatic drainage goes to the para-aortic lymph nodes, so they were examined and had an ultrasound scan which were both normal. Blood cultures grew Staphylococcus aureus and, after discussion with the microbiologist, an MRI spine was performed to rule out osteomyelitis. This showed L2/L3 osteomyelitis, epidural abscess and psoas inflammation (Fig. 1). The microbiologist also advised for a trans-oesophageal echocardiogram to rule out development endocarditis, which was normal. On further questioning, the patient had acupuncture treatment 2 weeks prior to admission for mechanical back pain. The treatment was performed by a trained physiotherapist and involved the insertion of sterile disposable needles into acupoints in the lower back to relieve pain.
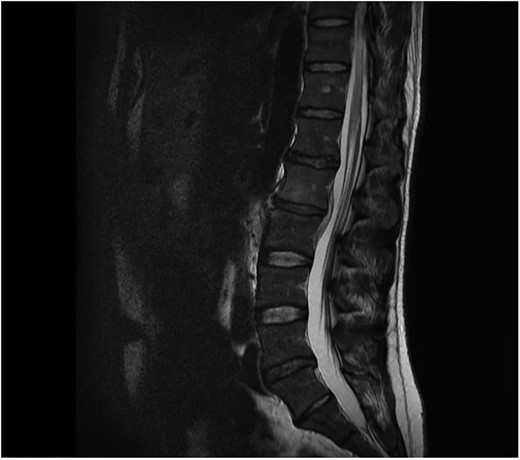
Sagital T1 MRI lumbosacral spine. Osteomyelitis in L2 and L3 vertebral bodies, epidural abscess and inflammation of the psoas muscles.
Neurosurgical advice recommended that due to the lack of neurological symptoms the patient could be treated conservatively with antibiotics. Microbiology advice was to treat the patient with IV flucloxacillin and oral rifampicin for at least 2 weeks and then to continue with oral antibiotics for at least a further 6 weeks depending on clinical improvement. Repeat bloods and MRI scans were performed to monitor the response to antibiotics (Fig. 2).
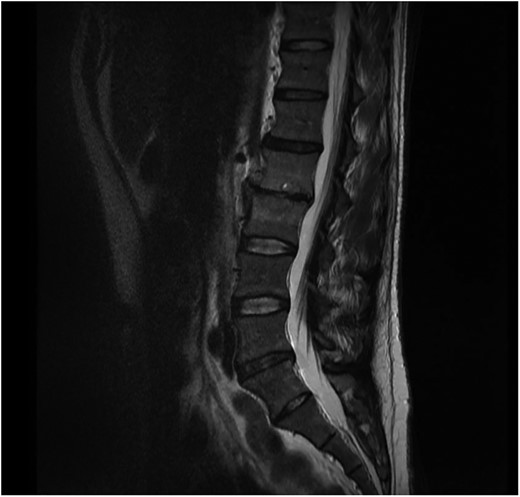
Sagital T1 MRI lumbosacral spine. 2 months later the epidural abscess has resolved and minimal marrow oedema is seen in L2 and L3 vertebra.
The patient completed a 2-week course of IV antibiotics followed by a further 12-week oral course. The patient responded well to antibiotic therapy as evidenced by normal inflammatory markers and resolution of osteomyelitis and epidural abscess on MRI.
DISCUSSION
Acupuncture has developed in China over thousands of years. It has been more commonly used in the West especially for low back pain. This case highlights a rare but potentially severe complication of acupuncture. Major complications are rare, having an incidence of 0.55 per 10 000 patients according to one study [1]. Common risks of acupuncture include local cellulitis and rarer complications of neurovascular damage and pneumothorax have been reported [1].
Spinal epidural abscess is a rare condition accounting for 1 per 20 000 hospital admissions [2]. Predisposing risk factors for developing an epidural abscess include diabetes mellitus, chronic kidney disease, an immunocompromised status, trauma, surgery, nerve acupuncture and infection (i.e. sepsis, soft tissue infection, osteomyelitis and urinary tract infection) [3].
Only six cases of spinal epidural abscess formation following acupuncture have been published [3–7]. The majority of these cases are reported in China, Japan or Korea where acupuncture use is most common but this is the first reported case in the UK. Five of these cases were treated successfully with an extended course of antibiotics and serial MRIs with one case requiring total laminectomy of L3–4. Five patients had a full neurological recovery and one had paraplegia with no improvement. The most common causative pathogen is Staphylococcus aureus, which accounts four of these cases the others being Serratia marcescens and Escherichia coli.
Although spinal epidural abscess is an uncommon disease in this case a complete history would have highlighted recent acupuncture usage and would have led to a quicker diagnosis. As acupuncture becomes more commonly used doctors should be aware of the potential benefits and complications to their patients.
CONFLICT OF INTEREST STATEMENT
None declare.



