-
PDF
- Split View
-
Views
-
Cite
Cite
Yu-Min Su, Chih-Hsuan Changchien, Self-inflicted, trans-optic canal, intracranial penetrating injury with a ballpoint pen, Journal of Surgical Case Reports, Volume 2016, Issue 3, March 2016, rjw034, https://doi.org/10.1093/jscr/rjw034
Close - Share Icon Share
Abstract
Trans-orbital penetrating injuries are not common. If not promptly treated, these injuries can lead to serious disabilities and even death. A 60-year-old man, who had multiple underlying diseases, was admitted to our medical ward for the treatment of aspiration pneumonia; he attempted suicide by inserting a ballpoint pen into his left eye. CT of the brain showed a foreign body penetrating through the left optic canal into the intracranial parasellar region without obvious intracranial haemorrhage. The foreign body was withdrawn smoothly at bedside without a craniotomy. The patient was then transferred to the ICU for neuro-observation. The patient recovered with complete left ophthalmoplegia but intact visual function. Acute management of a trans-orbital penetrating injury involves prompt neuroimaging examinations and knowledge of common recurring patterns of injury. All clinicians should be aware of the psychological condition of each patient, and suicide precautions should be considered during clinical practice.
INTRODUCTION
There have been few reports in the literature regarding trans-orbital penetrating injuries from a non-missile, low-velocity object; these incidents are usually caused by violence, accidents or suicide attempts [1]. A penetrating object of >5 cm in length could reach the cranial cavity through the orbital roof or the superior orbital fissure. An intracranial penetrating injury through the optic canal is extremely rare [2]. Self-inflicted penetrating brain injuries from a ballpoint pen have only been discussed in a few case reports [3]. In this report, the author reviews a case of a self-inflicted, trans-optic canal, intracranial penetrating injury that was inflicted with a ballpoint pen in a medical setting.
CASE REPORT
A 60-year-old man was admitted to our medical ward due to aspiration pneumonia. He had a medical history of diabetes mellitus, end-stage renal disease; a tuberculosis bacilli-related thoracic spine infection with paraplegia, and a previous coronary artery bypass graft. During his third day at the hospital, he obtained a ballpoint pen and inserted it into his left eye. On physical examination, the patient appeared to be alert with normal vital signs. The ballpoint pen protruded from his left upper eyelid; it was firmly lodged in his left medial orbit between the globe and nose, causing left eye proptosis (Fig. 1). Neurologic examinations revealed that the patient was neurologically intact except for complete left ophthalmoplegia. Brain CT scanning revealed a tubular foreign body that was located in the anteroposterior plane extending from the orbital apex and directly into the parasellar region (Fig. 2). The metallic portion of the foreign body was entrapped in left optic canal (Fig. 3). There was no evidence of intracranial hemorrhaging or a rupture in the globe (Fig. 4). The patient was treated with high-dose steroids to protect the optic nerve. The plastic ballpoint pen and metallic tip was withdrawn from the orbit smoothly at bedside, and no craniotomy was required. The ballpoint pen had been inserted to an estimated depth of 7 cm through the eyelid and into the orbit. The patient was then transferred to the ICU for close neuro-observation. We initiated intravenous broad-spectrum antimicrobials and vancomycin therapy and continued these medications for three weeks. A psychiatrist was consulted for a complete psychiatric evaluation and suicide prevention. The follow-up CT scan showed no retained foreign bodies or intracranial hemorrhaging (Fig. 5). At the last follow-up examination 2 months after the injury, the patient presented with complete left ophthalmoplegia and blepharoptosis but intact visual function.

The ballpoint pen was firmly lodged in his left medial orbit between the globe and nose.
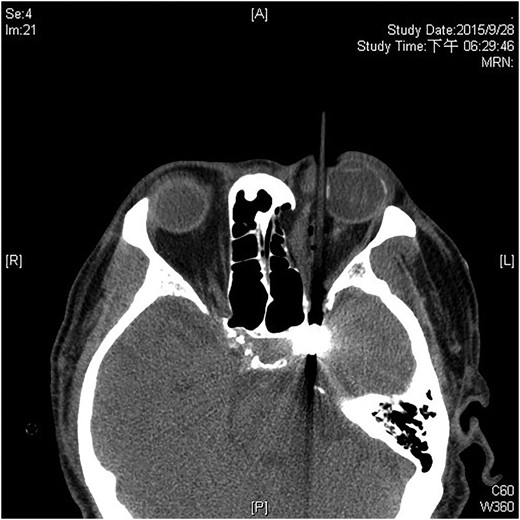

The ballpoint pen tip reaches into the parasellar region via the optic canal.
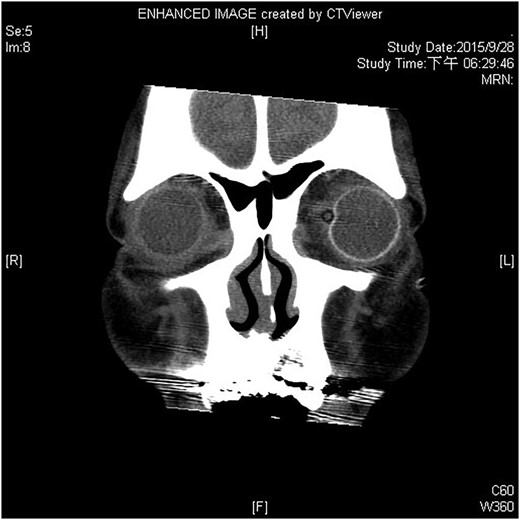

The follow-up CT scan shows residual hematoma in the orbital cavity; no retained foreign bodies or intracranial hemorrhaging.
DISCUSSION
Self-inflicted eye injuries are not unusual in psychiatric patients. However, these types of injuries rarely occur in medical settings. Medically-ill patients are more likely to attempt suicide by jumping or by hanging or cutting. Numerous psychodynamic and biochemical theories exist to explain self-inflicted eye injuries, which can range from autoenucleation to severe trans-orbital, intracranial penetrating injuries [4]. If not treated promptly, these injuries can result in serious neurologic damage or even death.
Brain and face CT scans are the primary modalities used in the neuroimaging examinations of patients with intracranial penetrating injuries. MRI is generally not recommended for use in the acute management of penetrating brain injuries, because it can be potentially dangerous in cases of retained ferromagnetic objects due to possible object movement in response to magnetic torque [5]. However, MRIs can be useful if a wooden object caused the penetrating brain injury. Cerebral angiography, CT angiography or MR angiography can be used when there is evidence of possible vascular or cavernous sinus injury. Embolization and proximal and distal control of the carotid artery prior to the removal of the foreign body allow for rapid control of any hemorrhage.
Reports about intracranial penetration via the orbit with various types of foreign bodies have been published [6]. Occasionally, the eye is spared remarkable injury due to the tough scleral coat and the motility of the globe [7]. An intact globe or the absence of focal neurologic deficits dose not excludes the presence of a lethal intracranial trauma.
The surgical indications following penetrating orbital injuries are retained foreign bodies, cerebrospinal fluid leakage immediately after a trauma, displaced bone fractures, intracranial hematomas and evidence of direct vascular injury. In the majority of cases, foreign body removal and neurovascular decompression can be accomplished by a craniotomy around the wound. However, non-operative management has been successful in several case reports, depending on the nature of wounding instrument [8]. Patients that sustain intracranial penetrating injuries and nondisplaced orbital fractures without bone fragments and that have no evidence of any brain parenchymal injury may undergo a removal of an externally accessible foreign body without a craniotomy. However, this process should not be taken as the standard treatment recommendation for similar situations. The removal of a penetrating foreign body outside the operating room may lead to life-threatening hemorrhage in rare cases.
Abscesses typically develop within 3–5 weeks after injury, with Staphylococcus aureus being the most common organism. However, gram-negative bacteria also frequently cause intracranial infection after injury. Whenever an intracranial abscess develops, a retained foreign body should be suspected. It has been recommended that broad-spectrum antimicrobials should be prescribed in all penetrating brain injury cases for at least 7–14 days [1].
In our patient, the injury had resulted in a complete left ophthalmoplegia and blepharoptosis at the 2-month follow-up. However, in a reported series of 33 patients with traumatic superior orbital fissure syndrome, majority of patients had regained moderate extraocular muscle function in all three cranial nerves at the 6-month follow-up visit [9].
Inpatient suicide among medically-ill patients is a relatively rare event that is often difficult to predict and prevent. Traditional risk factors such as a history of psychiatric illness, substance abuse or suicidal tendencies may not be typically present in medical/surgical patients at risk for suicide-attempts. Constant surveillance of agitated patients at risk for suicide-attempts and planned interventions to calm them, along with securing their surroundings may be beneficial prediction and prevention approaches [10].
CONFLICT OF INTEREST STATEMENT
None declared.



