-
PDF
- Split View
-
Views
-
Cite
Cite
Ayman Khalil, James Clerkin, Tafadzwa Mandiwanza, Sandra Green, Mohsen Javadpour, Unilateral abducens and bilateral facial nerve palsies associated with posterior fossa exploration surgery, Journal of Surgical Case Reports, Volume 2016, Issue 3, March 2016, rjw028, https://doi.org/10.1093/jscr/rjw028
Close - Share Icon Share
Abstract
Multiple cranial nerves palsies following a posterior fossa exploration confined to an extradural compartment is a rare clinical presentation. This case report describes a young man who developed a unilateral abducens and bilateral facial nerve palsies following a posterior fossa exploration confined to an extradural compartment. There are different theories to explain this presentation, but the exact mechanism remains unclear. We propose that this patient cranial nerve palsies developed following cerebrospinal fluid (CSF) leak, potentially as a consequence of rapid change in CSF dynamics.
INTRODUCTION
Cranial nerve palsies can result as a complication of posterior fossa procedures involving or adjacent to the brain stem. A number of case reports in the literature have described multiple cranial nerve palsies secondary to neurosurgical interventions with resultant brain stem injury [1, 2]. We report a rare case of a unilateral abducens and bilateral facial nerve palsies following a posterior fossa exploration confined to an extradural compartment.
CASE REPORT
A 39-year-old male had resection of a left cerebellar hemangioblastomas on 12 May 2015. He presented to the emergency department on 7 July 2015 with a 10-day history of fever, fatigue and dizziness. His temperature on presentation was 38.7°C, with normal serum white cell count and C-reactive protein. A pre and post contrast computed tomography (CT) of the brain showed no evidence of infective collection. Lumbar puncture resulted in a leukocyte count of 253 cells/µl (65% polymorphs), with no causative organism. Peripheral blood cultures were sterile. He was commenced on vancomycin [15 mg/kg bd—titrate based on levels, cefotaxime (2 g qds) and metronidazole (500 mg tds)]. Despite broad spectrum cover, he continued to have regular pyrexic episodes. Multiple septic screens, including lumbar puncture, failed to yield a source. With input from microbiology service, it was felt that the bone flap could be the proposed focus of infection. He underwent reopening of posterior fossa craniotomy wound and removal of bone flap on 21 July 2015. The surgery was confined to the extradural compartment, although there was cerebrospinal fluid (CSF) loss during the surgery. The bone flap was cultured and sent for polymerase chain reaction (PCR). No infective aetiology was detected. Following the surgery, the patient developed bilateral facial and a left abducens nerve palsy. His temperature settled post removal of the bone flap, and his antibiotics were stopped on 27 July 2015.
Examination revealed bilateral lower motor neuron facial nerve palsies, House Brackmann grade 4 bilaterally. Functional assessment noted mild slurring of speech. Examination of the other cranial nerves revealed left abducens nerve palsy. Power in all limbs was normal, with normal deep tendon reflexes, and his sensory examination was unremarkable. There was moderate ataxia on gait examination.
Magnetic resonance imaging (MRI) of the brain performed Day 2 post procedure showed fluid-attenuated inversion recovery sequence (FLAIR) abnormality within the floor of the fourth ventricle, on the dorsal pons, involving the facial colliculus (Fig. 1).
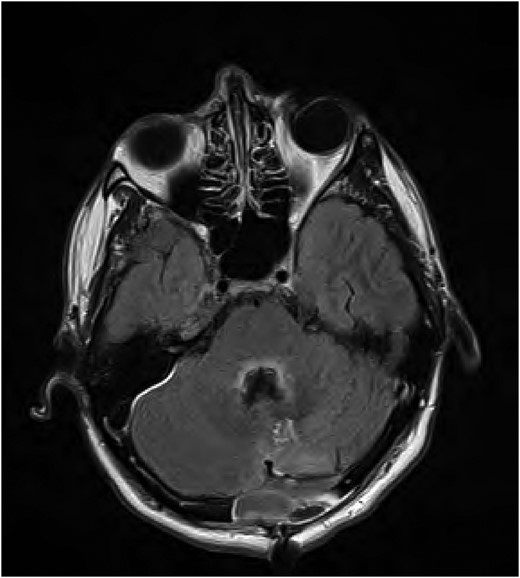
FLAIR MRI brain showing high signal abnormality in the floor of the fourth ventricle.
He was reviewed by the ophthalmology team which confirmed the examination findings and advised eye patch and moisturizing eye drops. The patient had a repeat MRI brain on 11 August 2015 which showed interval decrease in the focal hyperintensity surrounding the fourth ventricle and dorsal pons (Fig. 2). He was subsequently discharged from the hospital. On review in clinic on 11 November 2015, there had been significant improvement in his sixth cranial nerve function, but there was no improvement in his bilateral facial palsies.
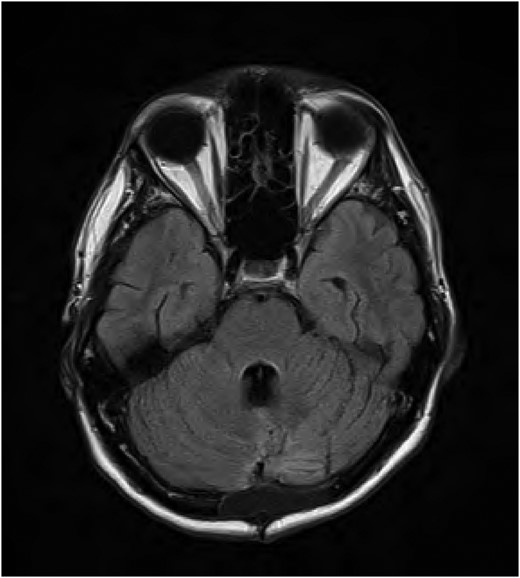
FLAIR MRI brain follow-up showing improvement of the signal abnormality in the fourth ventricle.
DISCUSSION
The differential diagnosis for multiple cranial neuropathies is vast. Treating physicians must out rule congenital, traumatic, infective and neoplastic causation. Idiopathic aetiology remains a frustrating diagnosis of exclusion [3]. Mixed cranial nerve palsies are an infrequent observation in minor neurosurgical operations, particularly those involving both the facial and the abducens nerves. However, their proximity at the pontomedullary junction leaves them susceptible to compressive effects.
A possible anatomical hypothesis for dual abducens and facial nerve palsies lies in their relative intracranial courses. The abducens nerve has a delicate course through Dorello's canal on its way to the cavernous sinus, making it liable for traction injury imposed by the caudal descend of the cerebellum [4]. The same traction forces may result in impairment of the blood supply to the facial nerve. This is mainly secondary to displacement of the vascular network on the ventral side of the pons with subsequent hypoperfusion [5].
Bilateral abducens palsies after posterior fossa tumours, lumboperitoneal shunts and meningeal alterations of the foramen magnum surrounding tissues have been reported previously [5]. All these conditions result in caudal displacement of the parenchyma after CSF leakage. In the aforementioned case, CSF drainage during the surgery may be considered one possible mechanism for development of his postoperative cranial nerve palsies. However, the intraoperative CSF leak would have been as expected. and the patient was in the prone position intraoperatively and lying in bed postoperatively which would make significant cerebellar and brainstem sag unlikely. Direct compression of the facial and abducens nerves against a clivo-axial angle due to the pontomedullary junction effacement is another potential mechanism for these unusual clinical sequelae, but there was no imaging evidence of this on the MRI scans. The exact mechanism for development of postoperative cranial nerve palsies and the FLAIR high signal in the floor of the fourth ventricle in our patient remains unclear.
In conclusion, Patients presenting with mixed cranial neuropathies necessitate urgent radiological and clinical assessment. Cranial nerve palsies can develop following CSF leak, potentially as a consequence of rapid change in CSF dynamics. We are reporting a rare unilateral abducens and bilateral fascial palsies following a minor posterior fossa exploration surgery.
CONFLICT OF INTEREST STATEMENT
None declared.



