-
PDF
- Split View
-
Views
-
Cite
Cite
Masatoshi Adachi, Yusuke Miyata, Yuki Ito, Mid-facial deformity secondary to a traumatic haemorrhage in a maxillary cyst, Journal of Surgical Case Reports, Volume 2016, Issue 2, February 2016, rjw013, https://doi.org/10.1093/jscr/rjw013
Close - Share Icon Share
Abstract
Serious symptoms caused by intra-cystic bleeding are very rare. We describe a case of a maxillary cyst presenting with mid-facial deformity in a Japanese woman. She underwent bilateral Caldwell–Luc procedure 21 years earlier and suffered left cheek trauma 4 years earlier. She presented soon after the trauma complaining of left mid-facial deformity, and computed tomography showed a trilocular cystic lesion in the left maxilla. We performed facial osteotomy concurrent with cyst enucleation with lateral rhinotomy. Serosanguineous fluid filled the cyst cavity just below the face; however, additional cyst cavities contained straw-coloured fluid. She showed no signs of recurrence at the end of a 20-month follow-up, and her postoperative appearance was excellent. Histopathological examination showed that all cyst walls were lined by ciliated columnar epithelium, which was consistent with surgical ciliated cyst. We consider that the increased intra-cystic pressure caused by traumatic haemorrhage induced expansion of the pre-existing surgical ciliated cyst.
INTRODUCTION
Very rarely, haemorrhage caused by trauma or bleeding tendency forms cyst-like lesions in the potential space surrounding vessels [1]. In the oral and maxillofacial region, these lesions are known by a variety of names, including traumatic bone cyst, solitary bone cyst and simple bone cyst, and intramedullary haemorrhage of the jaw is the most accepted pathogenetic theory [2]. Most cases of maxillofacial haemorrhagic bone cysts are asymptomatic and do not cause expansion of the cortical bone; however, expansion of the maxillofacial cyst caused by intra-cystic bleeding presents with serious symptoms. A case of mandibular cyst causing paraesthesia of the mental region has been reported [3]. This incidental clinical state was caused by spontaneous haemorrhage into the pre-existing cyst.
We report a case of maxillary cyst presenting with mid-facial deformity where the patient had previously undergone maxillary sinus surgery and later suffered trauma of the cheek region. We also discuss the pathogenesis of this unusual case and the outcome of our treatment.
CASE REPORT
A 44-year-old Japanese woman presented with a mid-facial deformity. Epilepsy was diagnosed, and her history included bilateral Caldwell–Luc surgery 21 years earlier and trauma to the left cheek region 4 years earlier. She presented soon after the trauma complaining of left mid-facial deformity. Nasal endoscopic surgery was performed 2 years after the injury, by an otolaryngologist, but her symptoms persisted after the surgery.
Physical examination revealed a non-tender, hard swelling of the left nasal wing from which serosanguineous fluid was aspirated by fine needle (Fig. 1). Intraoral examination showed a soft palatal expansion and on panoramic radiography, the identified cyst had no relation to the neighbouring teeth. Computed tomography showed a trilocular cyst in the left maxillary region (Fig. 2). A clinical diagnosis of surgical ciliated cyst was made, and facial osteotomy and cyst enucleation were performed under general anaesthesia. Lateral rhinotomy provided excellent exposure of the expanded cortical bone, which was removed carefully with a bone chisel. Serosanguineous fluid filled the cyst cavity just below the surface; however, palatal and nasal cyst cavities contained straw-coloured fluid. The cyst was enucleated, and the facial wound was closed primarily (Fig. 3). Healing was uneventful. Histopathological examination showed that all cyst walls were lined by ciliated columnar epithelium, which was consistent with surgical ciliated cyst (Fig. 4). The patient showed no signs of recurrence at the end of a 20-month follow-up, and the postoperative appearance was excellent (Fig. 5).

Appearance of the swelling in the left nasal wing at the initial examination.
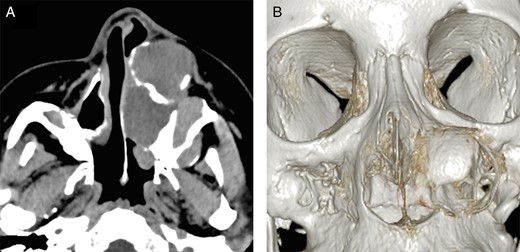
Computed tomographic appearance. (A) Axial computed tomographic section showed a well-defined trilocular cyst in the left maxillary region extending to the cortical plate. (B) Three-dimensional computed tomographic image showing a defect in the nasal lateral wall.
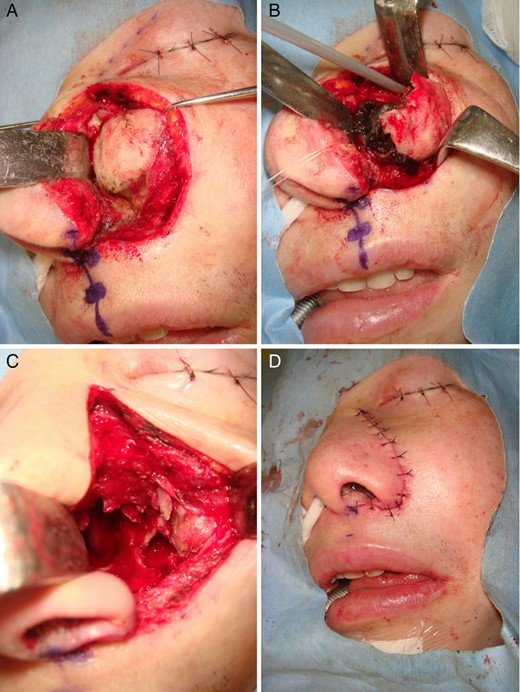
Operative findings in the case. (A) Lateral rhinotomy incision exposing the entire lesion. (B) Serosanguineous fluid filled the cyst cavity. (C) All cyst walls were enucleated. (D) The wound was closed primarily.
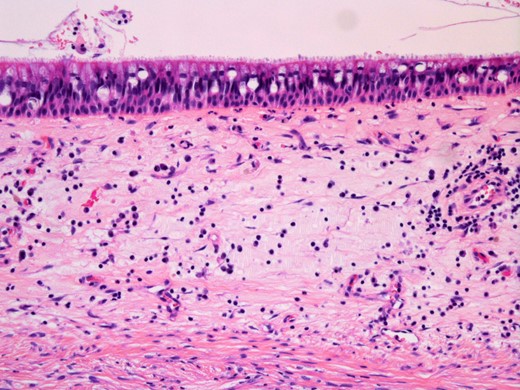
Histopathological findings of the cyst. Haematoxylin and eosin staining showing pseudostratified ciliated epithelium lining the cyst wall (original magnification ×200).

Postoperative appearance showing improvement of the facial deformity.
Informed consent was obtained from the patient's family to publish the details of her case, including photographs and other identifying information.
DISCUSSION
We report a unique case of a maxillary cyst that deformed the overlying mid-face, with buccal trauma as the initiating cause.
Based on the patient's history, it is obvious that the buccal trauma led to the lesion presenting as an unusual tumour. External injury can cause radicular cysts; however, in this case, the affected maxillary region was not related to the neighbouring teeth. Histopathology findings confirmed that all cyst walls indicated a surgical ciliated cyst, which is one of the most common maxillary cysts in Japan, and it can result from delayed complication of maxillary sinus surgery, trauma or infection [4]. In cases that follow radical sinus surgery, the initial presentation is typically expansion of vestibular or palatine bone cortical plates with only mild clinical abnormalities of the face. Because the patient had a previous history of bilateral sinus surgery and 19 years had passed since the maxillary surgical procedure, it seems reasonable that the surgical ciliated cysts were already present at the time of the initial cheek injury. The lesion consisted of three cavities, and only the facial portion was found to contain haematoid fluid, suggesting that the increased intra-cystic pressure caused by traumatic haemorrhage induced expansion of the lesion. To our knowledge, ours is the first report of maxillary haemorrhagic cyst augmentation presenting with mid-facial deformity. Although this is a secondary phenomenon, we consider this is a haemorrhagic cyst in the broadest sense.
There is fairly general agreement that marsupialization is an effective and less invasive treatment for surgical ciliated cyst; however, complete resolution followed by regeneration of normal bone requires an appreciable period [5]. In our case, immediate correction of the facial deformity was absolutely necessary; therefore, facial osteotomy concurrent with the cyst enucleation was considered the best approach. Usually, resection of maxillary cysts is similar to the technique and approach used with the basic Caldwell–Luc procedure, which is suitable for treatment of benign maxillary tumours, chronic empyema, fractures and exploration of the maxillary sinus; however, the Caldwell–Luc procedure provides an inadequate approach to the nasal cavity [6]. In our case, because the cyst extended to the middle meatus, good exposure of the nasal lateral wall was essential. The lateral rhinotomy approach allows wide access to the mid-facial region [7]. Wide exposure minimizes the surgical invasion, bleeding is readily controlled and the postoperative appearance is excellent.
We found that bleeding in a pre-existing maxillary cyst can potentially lead to expansion of the lesion and deformation of the face.
CONFLICT OF INTEREST STATEMENT
None declared.



