-
PDF
- Split View
-
Views
-
Cite
Cite
Fleur E.E. de Vries, Armin W. Walter, Bart C. Vrouenraets, Intraductal papilloma of the male breast, Journal of Surgical Case Reports, Volume 2016, Issue 2, February 2016, rjw014, https://doi.org/10.1093/jscr/rjw014
Close - Share Icon Share
Abstract
We report the case of a 29-year-old male patient who presented with a painless lump of his left breast that was found to be an intraductal papilloma. This is an extremely rare, but benign disease in the male breast. We subsequently discuss radiologic tests and treatment options.
INTRODUCTION
In contrast to the female breast, in which benign and malign diseases are relatively common, the male breast is not so often affected. However, also male patients can present with breast abnormalities. There is a wide differential diagnosis of a male breast lump comprising gynecomastia, fibroadenoma and lipoma. Next to this, more rare conditions should be considered like florid ductal hyperplasia, columnar cell lesions, ductal or lobular carcinoma in situ, intracystic papillary carcinoma and invasive breast cancer. An intraductal (or intracystic) papilloma (IP) is an extremely rare benign disease of the male breast. We describe the case of a healthy 29-year-old male patient with an IP of his left breast.
CASE REPORT
A 29-year-old male patient presented at the outpatient clinic with a painless palpable lump. Four years before, he had consulted his family doctor because of a swollen left breast. Ultrasonography at that time demonstrated gynecomastia (BIRADS II), probably due to (mis)use of anabolic steroids. At presentation, he had a persisting swollen left breast with a rounded palpable mass under his nipple, which was mildly painful on palpation. He did neither longer use anabolic steroids nor any other medication. Our patient wanted the mass to be removed because of cosmetic reasons rather than his mild complaints. On clinical examination, we saw a healthy young man with a palpable 1-cm large tumor lateral under his left nipple.
Ultrasonography showed a long-shaped solid structure with lobular architecture. Additional mammography showed a lobulated structure behind the nipple with a diameter of ∼1.5 cm without microcalcifications (BIRADS III). Histological and immunohistochemical examination of a core needle biopsy demonstrated an intraductal proliferation compatible with an IP. Subsequently, surgical excision of the lump was performed under general anesthesia. Microscopy of the resected specimen confirmed the diagnosis of an IP of ∼1 cm with a free margin of <1 mm. Sections through preexistent breast tissue showed central dilatated cystic structures with a papillary proliferation of epithelial cells with partly cylindrical morphology and heterogenous (non-monotonous) appearance. We found no indication of invasive growth (Figure 1). Immunohistochemistry showed 10% MIB-1 activity. SMA and keratin 5/6 staining demonstrated the presence of myoepithelial cells throughout the lesion with a heterogenous random staining pattern in the keratin 5/6 slide supporting the diagnosis of a benign proliferation (Figure 2).
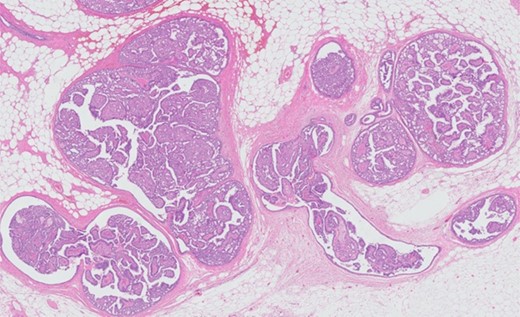
Hematoxylin and eosin stain (HE) overview. HE microphotograph with an overview of the lesion characterized by cystic and papillary architecture. No indication of invasive growth.
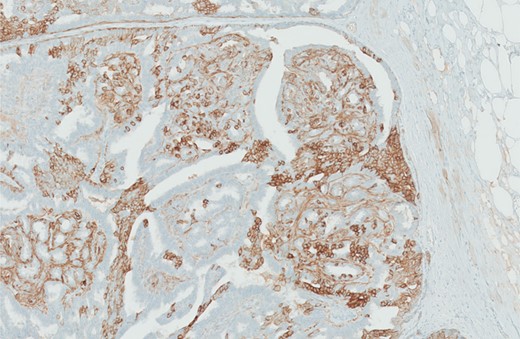
SMA and keratin 5/6 immunohistochemistry demonstrates the presence of myoepithelial cells throughout the lesion with a heterogenous random staining pattern in the keratin 5/6 slide supporting the diagnosis of a benign proliferation.
DISCUSSION
We described the case of 29-year-old healthy male patient with an IP of his left breast. In contrast to an intraductal papillary carcinoma or an invasive papillary carcinoma, an IP is a benign disease. The clinical presentation is a painless or painful subareolar mass, with or without nipple discharge. An IP can present at any age [1–4]. Radiologic diagnostic tests involve ultrasonography (with fine needle aspiration and needle biopsy) and mammography. Magnetic resonance imaging (MRI) can be performed supplementary. A study of Sarica et al. [5] on MRI for papillary breast lesions concluded that the major benefit of retroareolar imaging appears to arise from its ability to demonstrate ductal relation and extension of contrast-enhanced regions. Using immunohistochemistry for pathological diagnosis is very important to distinguish between an IP and a papillary carcinoma. Once diagnosed, both conservative (close follow-up) and operative (surgical excision) are possible. A study of Lam et al. [6] concluded that the radiologic features are not sufficiently sensitive or specific to differentiate benign from malignant papillary lesions and emphasized the need of surgical excision. Contrarily, a study of Sydnor et al. [7] found that benign papillomas diagnosed at core biopsy are infrequently (3%) associated with malignancy, and therefore mammographic follow-up seems reasonable. Swapp et al. [8] also described that in the case of a core biopsy-proven benign lesion, follow-up is justified and excision is not necessary. They emphasized that because of the high association with malignancy (67%), diagnosis of atypical papilloma at core biopsy should prompt excision for definitive diagnosis. When surgical treatment is performed, local excision of the lesion should be curative. Recurrence of the IP after local excision was only described once [3]. Overall, prognosis is excellent.
In conclusion, IP in the male breast is an extremely rare benign disease. The lesion can be treated by simple local excision or close follow-up.
CONFLICT OF INTEREST STATEMENT
None declared.



