-
PDF
- Split View
-
Views
-
Cite
Cite
Grace W. Ma, Andrew Yuen, Paraskevi A. Vlachou, Sandra de Montbrun, An unconventional therapeutic approach to a migratory IUD causing perforation of the rectum, Journal of Surgical Case Reports, Volume 2016, Issue 2, February 2016, rjw004, https://doi.org/10.1093/jscr/rjw004
Close - Share Icon Share
Abstract
Intrauterine devices (IUDs) are a commonly used form of contraception. The risk of perforation and migration of these devices have been reported to be 1 in 1000. Migration into the rectum is even more uncommon. The following case illustrates a previously healthy 37-year-old woman who experienced a perforation and migration of an IUD into the rectum necessitating endoscopic removal. To our knowledge, this complication of IUD and subsequent endoscopic removal has not been previously described and presents a viable first-line therapeutic option in a stable patient.
INTRODUCTION
The intrauterine device (IUD) is a popular method of contraception with worldwide use approaching 15% [1]. It is, however, associated with an estimated uterine perforation rate of 1 per 1000 insertions [1, 2]. Various retrieval methods of migrated extra-uterine IUDs have been described in the literature including endoscopy, laparoscopy or laparotomy. The following case report outlines the endoscopic retrieval of a migrated IUD into the rectal lumen.
CASE REPORT
A 37-year-old woman had an IUD inserted 1 year after her only pregnancy. The patient experienced post-procedural bleeding. At her follow-up, the strings of the IUD were not visualized, which was suspicious for IUD migration. An attempt at laparoscopic retrieval was unsuccessful. A computed tomography (CT) scan showed migration of the IUD with the T-arms of the device seen posterior to the left vaginal fornix with the shaft within the lower rectum (Fig. 1). A general surgeon was subsequently consulted, and a diagnostic flexible sigmoidoscopy was performed, which demonstrated protrusion of the IUD into the rectal lumen. The patient was then referred to a colorectal specialist.
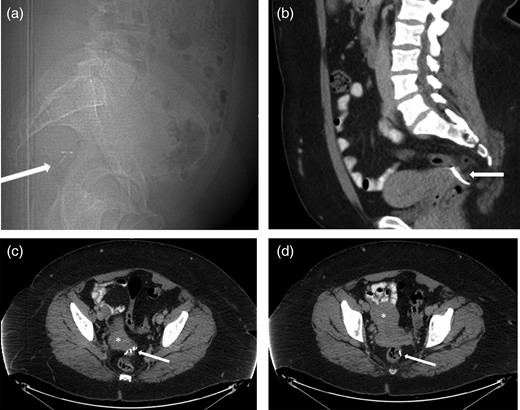
(a) Sagittal CT Scout view shows IUD (arrow) in very posterior location, probably within the rectum. (b) Sagittal contrast-enhanced CT of the pelvis showing the extra-uterine position of the contraceptive device (arrow) posterior to the uterus. (c) Axial contrast-enhanced CT of the pelvis reveals extra-uterine position of the contraceptive device arms (arrow) posterior to the cervix (*). (d) Axial contrast-enhanced CT of the pelvis showing the extra-uterine position of the stem of the contraceptive device within the rectal lumen (arrow) after perforating the uterus (*).
An magnetic resonance imaging (MRI) performed 1 month following the original CT demonstrated the T-arms of the IUD to have migrated within the rectum ∼10–12 cm above the anorectal junction at or just above the peritoneal reflection.
At this point, the patient was relatively asymptomatic except for non-cyclical painless bleeding. She was consented for transanal IUD extraction with the possibility of a laparoscopic extraction and repair. The patient was brought to the operating room, given sedation and positioned in left lateral decubitus for endoscopic extraction. A flexible gastroscope was advanced to the level of the T-arms which were caught proximal to a rectal fold. The arms were grasped with alligator forceps and manipulated in a proximal direction to dislodge the device. Once the entire IUD was free, the stem was pulled distally and removed transanally. The scope was then reinserted, and the rectal wall appeared healthy with no evidence of intraabdominal perforation. The patient tolerated the procedure well and was discharged home after an overnight observation period.
A follow-up CT was performed on Postoperative Day 2 with rectal contrast showing no extravasation of contrast to suggest a leak. The patient was subsequently discharged from hospital without complication.
DISCUSSION
Many IUD-associated uterine perforations are asymptomatic, and the actual incidence may be higher than reported [3]. Although uterine perforation may be painless, migration into the gastrointestinal tract may present as chronic lower abdominal pain, fever or diarrhea [3].
Early retrieval is recommended for extra-uterine IUDs [3] because of the risk of fistula formation and colon perforation [3]. Endoscopy, laparoscopy and laparotomy are described methods of retrieval. Removal of an IUD using endoscopy has been described in cases of migration through the lower rectum [4] and colon [5], but there has been no previous report of perforation in the upper rectum to our knowledge. The benefit of an endoscopic approach as first-line therapy is the avoidance of an operation that could require extensive dissection to the lower rectum with risk of injury to pelvic nerves and vasculature [4]. If the IUD is amenable to endoluminal retrieval, this approach may also prevent the need for a colotomy (and primary repair) or resection (and anastomosis or stoma) in order to remove the IUD [5, 6].
Penetration of the rectal lumen is an uncommon complication of IUD migration after uterine perforation. Removal of the IUD is recommended and can be performed endoscopically with proper technique and preoperative planning. This case describes the successful retrieval of an intraluminal IUD using careful endoscopic manipulation to extract the device without further injury to the rectal wall.
CONFLICT OF INTEREST STATEMENT
None declared.



