-
PDF
- Split View
-
Views
-
Cite
Cite
Edward J. Woo, Ross A. Ogilvie, Van Schaumburg Krueger, Michael Lundin, David M. Williams, Iliac vein compression syndrome from anterior perforation of a pedicle screw, Journal of Surgical Case Reports, Volume 2016, Issue 2, February 2016, rjw003, https://doi.org/10.1093/jscr/rjw003
Close - Share Icon Share
Abstract
May–Thurner syndrome is an anatomic variant where the right common iliac artery compresses the left common iliac vein. The variant exists in a significant portion of the population, but is usually asymptomatic; however, clinically significant stenosis can occur by iatrogenic means. In this report, we describe a patient who presents with left lower extremity pain and swelling. Initial workup for deep vein thrombosis was negative. After being referred to our venous clinic, a magnetic resonance angiography revealed narrowing of the left common iliac vein with a tortuous right common iliac artery crossing over the constriction. During left iliac vein stent placement, a pedicle screw from a prior L2–S1 spinal fusion was noted to be perforated through L5 vertebral body impinging the posterior aspect of the vein. This case demonstrates that increased scrutiny must be applied when dealing with pathology in close proximity to any implanted medical device.
INTRODUCTION
Iliac vein compression syndrome (IVCS) is most commonly due to May–Thurner variant, an anatomic variant wherein the right common iliac artery overlies the left common iliac vein and compresses it against the lumbar spine [1]. One study estimates that 24% of the US population has this variant, which is defined as 50% luminal constriction of the left common iliac vein, and all patients were asymptomatic [2]. The incidence of a May–Thurner variant developing symptomatic IVCS from a perforated pedicle screw is not known, but presumably very low. Herein, we present a patient with probable May–Thurner variant anatomy who developed near complete occlusion of the left common iliac vein due to the compression by a perforated pedicle screw.
CASE REPORT
A 65-year-old woman presented with worsening left lower extremity pain and swelling. She had a long history of superficial varicosities and painful venous hypertension, previously treated with sclerotherapy and bilateral great saphenous vein ablations. These therapies provided her with partial relief, but she was still experiencing daily symptoms. Six years prior, she also had L2–S1 spinal fusion for degenerative joint disease. In the emergency department, she reported that she had woken up with severe pain and heaviness in her left leg from the knee down with her right leg being at baseline. Initial workup was negative for deep venous thrombosis, and after obtaining a magnetic resonance imaging (MRI) of the lumbar spine, her neurosurgeon did not think that the pain was related to her back. She then was referred to our venous clinic for further evaluation.
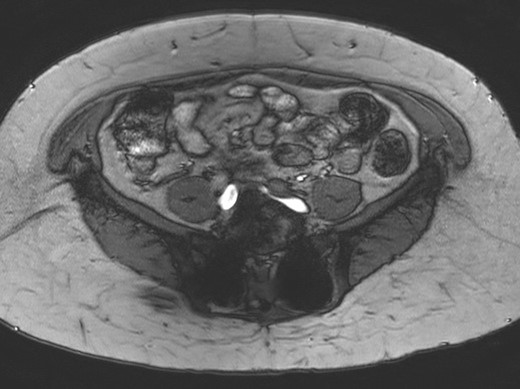
Vascular ultrasound of her left leg showed venous insufficiency in the small saphenous and Giacomini veins. Those findings were not severe enough to cause the level of discomfort that she was experiencing, so magnetic resonance angiography (MRA) of the pelvis was ordered. This study showed narrowing of the left common iliac vein to 0.2 cm (Fig. 1), with a tortuous right common iliac artery crossing over the constriction. The findings were consistent with non-thrombotic May–Thurner syndrome, which was thought to be the cause of her new symptoms.
The patient was scheduled for left iliac vein stent placement. During the procedure, impingement was noted upon the posterior aspect of the vein. At this location, there was perforation of a pedicle screw through the anterior cortex of her L5 vertebral body, from prior spinal fusion. This interaction was well visualized during intraluminal inflation of a 12 mm × 40 mm high-pressure balloon (Fig. 2) and was also seen after final stent placement (Fig. 3). Because the screw tip was completely unyielding, a 14 mm × 60 mm Wallstent was used instead of the 16 mm stent we typically use, so as to avoid undue compression of her overlapping right common iliac artery. After the procedure, the patient's symptoms were greatly improved. Follow-up venography performed 4 months postoperatively showed a patent stent with slight eccentric compression at the protruding screw and no evidence of in-stent stenosis.
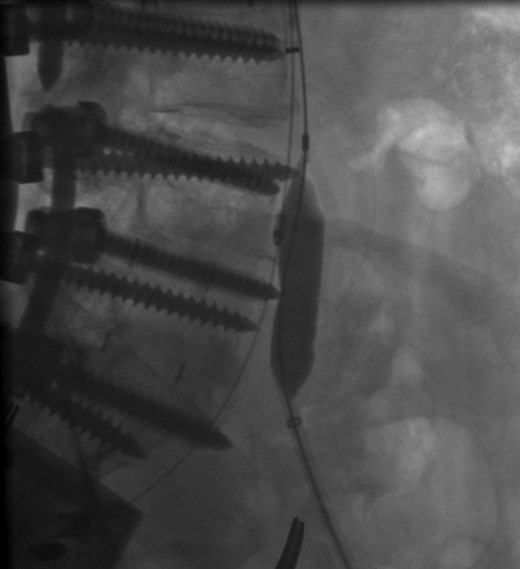
Perforation of a pedicle screw through the anterior cortex of L5 vertebral body visualized during intraluminal inflation of a 12 mm × 40 mm high-pressure balloon.
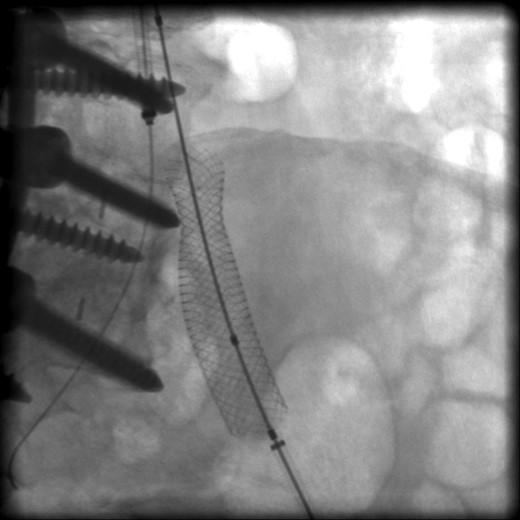
Intraoperative radiograph showing posterior compression of a wall stent within the left common iliac vein.
DISCUSSION
Perforation of the anterior vertebral cortex is a known complication of instrumented posterior spinal fusion with one study of 4790 pedicle screw insertions showing an incidence of 2.8% [3]. However, the level of risk caused by these perforations is thought to be very low. A literature review of 35 630 pedicle screw placements identified no patients with vascular compromise of any kind and only two visceral complications that were of clinical significance [4]. However, there are several documented reports of serious complications caused by anterior vertebral body perforation. Wegener et al. describe a case of penetration into the descending thoracic aorta [5]. O'Brien et al. outline a case of esophageal impingement caused by protruding pedicle screws at the T3 level [6]. Pre- and intraoperative radiographic modalities are necessary to decrease the risk of perforation [6].
Penetrations into the lung and ureter have also been documented [4, 7]. However, to our knowledge, this is the first reported case of iliac vein compression caused by pedicle screw perforation that has been reported. In this patient, the tortuous left common iliac artery probably did play a role by restricting the anterior movement of her left common iliac vein and causing the compression exerted by the screw to be more significant than anticipated. As in classic May–Thurner syndrome, we speculate that pressure from the screw produced chronic irritation of the vascular endothelium with resultant proliferation, thickening and stenosis explaining why her symptoms did not arise until 6 years after the hardware was placed [8]. Stent placement was chosen in this case because it was felt to be the most effective modality for restoring patency of the vessel. Pedicle screw impingement of the aorta has also been successfully corrected with endovascular stent placement [9]. However, in that case, they did elect to retract the screw as well [10]. Foxx et al. identified 33 patients with anterior cortical perforations that contacted major vessels [9]. Of these, two-thirds were in contact with an iliac vein. None of the patients studied went on to develop any sequelae as a result of vessel contact; thus, the authors of that article do not recommend repositioning of screws found to be in contact with a major vessel.
This case demonstrates the level of scrutiny that must be applied when dealing with pathology in close proximity to any implanted object. In our patient, neither lumbar MRI nor pelvic MRA was able to correctly identify a perforated pedicle screw as the cause of iliac vein compression. This is likely an exceedingly rare event, but the fact remains that standard imaging techniques are not always able to detect the interference of orthopedic hardware with essential internal structures.
Pedicle screw perforations are not uncommon, but they typically do not have any clinical ramifications. However, their proximity to major vessels and other vital structures makes them a potential cause of serious morbidity. This is more likely to occur in a patient who has a predisposition to pathology, such as May–Thurner syndrome. These susceptibilities may not be clinically obvious, so a high level of suspicion should be used whenever unexplained signs or symptoms arise in areas of prior orthopedic instrumentation.
CONFLICT OF INTEREST STATEMENT
None declared.



