-
PDF
- Split View
-
Views
-
Cite
Cite
David SC Soon, Hamish Shilton, Ali Andrabi, Mesothelial inclusion cyst: a rare occurrence, Journal of Surgical Case Reports, Volume 2016, Issue 12, 1 December 2016, rjw213, https://doi.org/10.1093/jscr/rjw213
Close - Share Icon Share
Abstract
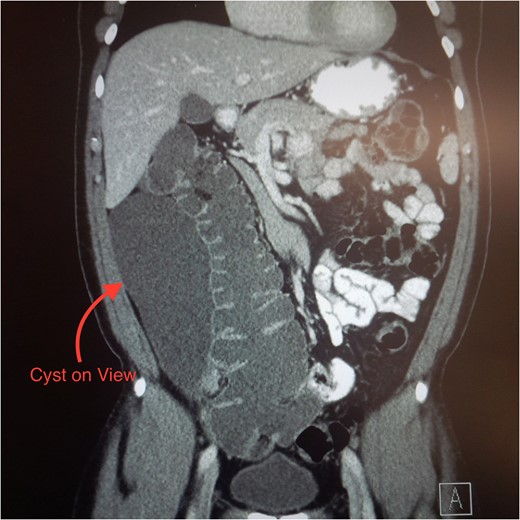
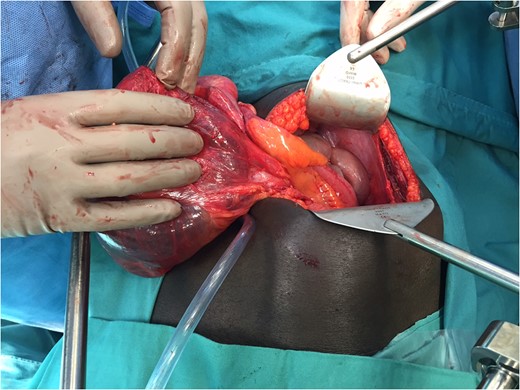
Mesothelial inclusion cyst is a rare benign tumour that has only 130 cases reported in the literature. Accurate diagnosis and optimal management of this condition remains uncertain. We report a 51-year-old African gentleman, whom presents with abdominal pain and constipation. A computed tomography scan was performed and revealed a large cystic lesion in the right paracolic gutter. The differential diagnosis included appendiceal mucinous neoplasm, cystic tuberculosis and duplication cyst. A laparotomy was performed due to his symptoms and size of the cyst. Macroscopically, the tumour had a size of 25 × 10 × 10 cm and revealed a necrotic lymph node. It was resected en bloc with the appendix and an ileocolic anastomosis performed. Histology revealed a diagnosis of mesothelial inclusion cyst and acute appendicitis. The patient recovered well and had no recurrence at 2-year follow-up.
INTRODUCTION
Mesothelial inclusion cyst is a rare tumour attached to the serosal surface of the visceral organs. It was initially thought to be cystic lymphangioma; however, electron microscopic examinations showed they originated from mesothelial cells [1]. Immunohistochemical markers such as calretinin also distinguish mesotheliomas from lymphangiomas. Whilst most mesothelial cyst reports are single cases, one study examining 37 cases found 84% presented in women of reproductive age with the remainder of either sex and of all ages [2]. The same report also noted that cysts were more frequently detected in patients who had previously had abdominal surgery or pelvic inflammation. We present an unusual case of a male patient who presented with acute appendicitis and an incidental mesothelial inclusion cyst.
CASE REPORT
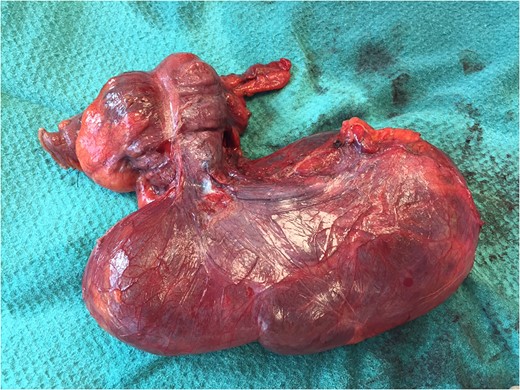
Histology revealed an inclusion mesothelial cyst lined by a single flattened layer of cells with bland ovoid to flattened nuclei and the cyst wall consisted of fibrous connective tissue. The cyst was confirmed as mesothelial by positive immunohistochemical reactions using cytokeratin-, AE1/3-, WT1- and calretinin-specific antibodies. Appendix histology revealed acute suppurative appendicitis containing an inflamed, perforated appendicular diverticulum.
The patient was well on initial follow-up. Four months postoperatively he complained of mild per rectal bleeding, but subsequent colonoscopy was normal with a well-healed anastomosis. On the annual follow-up, he is asymptomatic with no recurrent cystic tumour at 2 years.
DISCUSSION
Patients with mesothelial inclusion cysts usually present with a wide range of symptoms, including increasing abdominal girth, unspecific abdominal pain, nausea and vomiting [3]. Differential diagnoses to consider include: appendicitis, diverticulitis, Meckel's diverticulum, duplication cyst or cystic neoplasms [4]. CT scans and ultrasound visualize the lesion but do not differentiate from other intra-abdominal pathologies [5].
A paper by Lee in 2012 suggested that a laparoscopic approach proved to be superior to laparotomy and reduced length of stay, blood loss and complication rate. However, generally the risk of cyst rupture is higher in a laparoscopic approach than in an open approach [6]. As cystadenocarcinoma is a differential for cystic neoplasms of the appendix, rupture of any undifferentiated cyst associated with the appendix may place a patient at risk of pseudomyxoma peritonei [7]. Therefore, whilst laparoscopy may reduce early morbidity, a low threshold for conversion to open to facilitate safe dissection and avoid cyst rupture should be employed.
Mesothelial inclusion cysts were considered benign with excellent prognosis [8]. However, there is a high rate of recurrence, with an average of 32 months, and reports of neoplastic changes in this tumour. Whilst surgical intervention is considered the best approach for complete removal of cysts, recent studies advocate additional intraperitoneal chemotherapy to reduce recurrence but these remain preliminary, involving only a few patients [9]. If a cyst suggestive of a mesothelial cyst is found incidentally on imaging in an asymptomatic patient, suggested management would be for complete surgical excision and removal due to the small risk of malignancy as well as to exclude other differential diagnosis [8].
In conclusion, mesothelial inclusion cysts remain a rare intra-abdominal pathology. We suggest that a safe approach is total en bloc resection, keeping the cyst intact whether this is performed laparoscopically or through open approach, and lifelong follow-up to check for recurrence and/or neoplastic transformation.
ACKNOWLEDGEMENTS
We would like to thank Dr Vicky Tobin for final manuscript review and Peninsula Health staff for their assistance.
CONFLICT OF INTEREST STATEMENT
We would like to declare that there are no conflict of interest and no funding bodies for this study.



