-
PDF
- Split View
-
Views
-
Cite
Cite
Osamu Yoshino, Peter J. Prichard, Julian Choi, Old technique revisited with surgical innovation: complicated Mallory–Weiss tear with bleeding gastric ulcer exclusion, Journal of Surgical Case Reports, Volume 2016, Issue 1, January 2016, rjv173, https://doi.org/10.1093/jscr/rjv173
Close - Share Icon Share
Abstract
Mallory–Weiss tears (MWTs) rarely require surgical intervention. A 60-year-old female presented with massive hematemesis secondary to MWT and gastric ulceration. After failure of endoscopic management, an operative approach was embarked on, with a direct surgical hemostasis of the Mallory–Weiss tear and exclusion of the gastric ulcer. This exclusion strategy may be applicable for other patients with uncontrolled upper gastrointestinal bleeding in whom a simple repair would be difficult.
INTRODUCTION
Mallory–Weiss tears (MWTs) account for 6–14% of upper gastrointestinal bleeding (UGIB) [1]. Management of MWT generally consists of conservative measure and on occasion endoscopic intervention. Complicated MWT may rarely require surgical intervention for uncontrolled exsanguination [2].
CASE REPORT
A 60-year-old female was admitted for management of hematemesis. Three weeks prior, she sustained a flail chest, right hemothorax, splenic laceration, mesenteric injury, and lumbar and thoracic vertebral fractures in a motor-vehicle accident. She initially underwent a trauma laparotomy and right hemicolectomy. Significant hematemesis occurred 4 days after admission to the rehabilitation ward, and the patient was transferred to the intensive care unit (ICU), where a gastroscopy was performed. A large clot was observed in the fundus; however, there was no active bleeding. A Sengstaken–Blakemore (SB) tube was inserted and the gastric balloon inflated under endoscopic vision, and 6 units of packed red blood cells, 4 units of fresh frozen plasma, 2 units of platelets and 10 units of cryoprecipitate were transfused. Hemodynamic stabilization was achieved, and serum hemoglobin rose from 61 to 89 g/dl . A repeat gastroscopy the following day demonstrated the fundal clot plus a large MWT at gastroesophageal junction (GEJ) (Fig. 1). Adrenaline (1:10 000) was injected around the tear, and the SB tube was removed. The patient subsequently developed a pulmonary embolism, which was treated with an inferior vena caval filter. On Day 5 after transfer to the ICU, the patient was discharged to the regular ward. She was receiving proton pump inhibitor (PPI) therapy. Hematemesis recurred on Day 8, and the patient was intubated because of hemodynamic instability. Gastroscopy was performed after massive transfusion resuscitation, and the large fundal clot and MWT were again noted. Hemostatic powder (EndoClot®) was applied over the probable location of the fundal ulcer as well as MWT though there was no active bleeding.
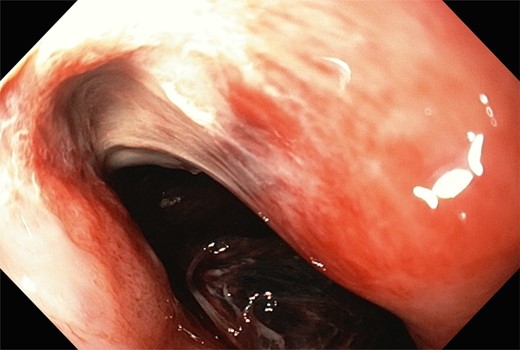
A large Mallory–Weiss tear and large fundal clot were observed during gastroscopy.
Gastroscopy the following day showed a fundal gastric ulcer and the MWT, which was now larger and deeper (Fig. 2). On Day 10, the patient underwent surgery. A midline laparotomy incision was performed, followed by extensive adhesiolysis. After the anterior wall of the stomach was exposed from the GEJ to pylorus, a longitudinal gastrotomy was created over the fundus. There was a deep MWT at GEJ extending along the greater curve of the stomach, which was bleeding actively. The MWT was oversewn with interrupted 3/0 PDS sutures and hemostasis achieved. A second, larger fundal ulcer, presumably from pressure necrosis of SB tube, was also noted. This ulcer occupied most of the fundus of stomach, which was excluded from the gastric cavity, by the closure of fundus with interrupted 3/0 PDS (Fig. 3). Postoperatively, oral fluids were commenced on Day 12. On Day 15, a Gastrografin swallow study was normal, and oral intake was encouraged. The patient recovered without complications and returned to the rehabilitation facility.
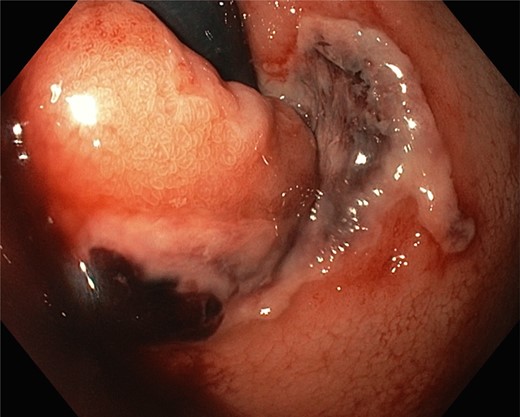
During the last gastroscopy, a fundal gastric ulcer and a larger and deeper Mallory–Weiss tear were noted.
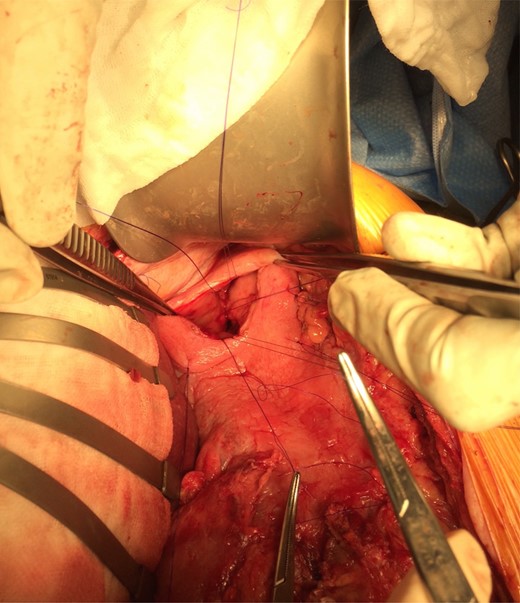
The gastric ulcer was excluded from the rest of the stomach through gastrostomy using 3/0 PDS suture.
DISCUSSION
UGIB is relatively common. Recent national audits from the UK and USA reported annual incidences of UGIB of 50–150 per 100 000 adults, with mortality rates of 2.5–10% [1, 3]. MWT is attributed to 5% of those patients. Generally, MWT is relatively common, and intervention is rarely required [4]. Currently, MWT is predominantly managed by observation and if necessary, gastroscopy and various advanced endoscopic techniques, including endoscopic diathermy, local adrenaline injections, local hemostatic agents, and endoscopic clips. Surgery is generally reserved for refractory bleeding and failed endoscopic management, and as such is rarely performed [5, 6]. In our patient, multiple endoscopies were performed with various techniques, including SB tube insertion, local adrenaline injection, bipolar electrocoagulation, and hemostatic powder (EndoClot®) application by our experienced gastroenterologist. Although SB tube was appropriately managed based on the institutional protocol, the MWT became complicated with a large gastric ulcer. Despite extensive efforts, bleeding remained uncontrolled and the Mallory–Weiss tear was perceived to be enlarging. Therefore, the MWT was directly sutured to achieve surgical hemostasis. Nevertheless, the second fundal ulcer due to SB tube posed a significant challenge because of its size and anatomical location.
Oversewing bleeding point of ulcer or ulcer excision are principles of surgical treatment and prevention for bleeding ulcer with the use of PPI [7]. In our case, MWT and associated ulcer was continuous and extensive and involved GEJ. Conventional surgical repair techniques seemed not feasible. The decision that a gastrectomy was deemed intolerable was due to difficult anatomy including adhesions and inflamed and fibrotic surrounding tissue, the clinical course, and the patient's compromised condition. The gastric ulcer exclusion that we performed in this case was the exclusion of ulcer internally from the gastric cavity with absorbable sutures. It was thought that hemostasis for refractory bleeding might have been achieved since it would have caused tamponade effects by itself, as well as protected from oral intake and acid production, combined with PPI.
Gastric exclusion was initially described by Waddell et al. in 1957, in the surgical treatment of duodenal ulcer. It involves subtotal gastrectomy to resect the antrum of stomach with vagotomy. Consequently, reduction in acid level appears to lead the healing of duodenal ulcer. Our exclusion technique is a different surgery, a temporary measure, potentially reversible and less physiologically demanding. It might be performed as an alternative to gastrectomy for UGIB.
Since the evolution of endoscopy and the advent of PPI therapy, the surgical management for UGIB has been almost completely substituted by the endoscopic interventions except for the rare event where hemostasis could not be achieved endoscopically [3]. This report describes, to our best knowledge, the successful performance of complex surgical management, including the first gastric ulcer exclusion, for recurrent bleeding from a MWT and associated ulcer. Furthermore, this case highlights not only the importance of conventional surgical technique and established knowledge but also the timely manner of surgical decisions in a physiologically complex patient. This exclusion strategy may be applicable for other patients with uncontrolled UGIB in whom a simple repair would be difficult.
CONFLICT OF INTEREST STATEMENT
None declared.



