-
PDF
- Split View
-
Views
-
Cite
Cite
Alisa M. Yee, Barbara G. Kelly, Juan M. Gonzalez-Velez, Eric K. Nakakura, Solid pseudopapillary neoplasm of the pancreas head in a pregnant woman: safe pancreaticoduodenectomy postpartum, Journal of Surgical Case Reports, Volume 2015, Issue 8, August 2015, rjv108, https://doi.org/10.1093/jscr/rjv108
Close - Share Icon Share
Abstract
Solid pseudopapillary neoplasms (SPNs) of the pancreas are rare and typically arise in young women. The optimal management of a pregnant woman suspected of having an SPN of the pancreas head is unclear. We report such a case where close monitoring for tumor growth was done during pregnancy and a successful pancreaticoduodenectomy was performed after term delivery.
INTRODUCTION
Solid pseudopapillary neoplasms (SPNs) of the pancreas typically arise in young women and are extremely rare [1]. Although SPNs have a low malignant potential, lymph node and distant metastases are found in 2 and 5–10% of cases, respectively [1]. They also can be locally invasive and spontaneously rupture. Therefore, surgical resection is recommended for fit patients [2].
A particular challenge is how best to manage a pregnant patient diagnosed with a pancreatic SPN. Progesterone receptors are consistently detected in SPNs, and progesterone levels rise dramatically during pregnancy [3]. Spontaneous rupture of a pancreatic SPN in a pregnant woman has been reported [3]; however, a direct link between elevated progesterone levels and tumor growth/rupture has not been established. But, concern for tumor growth and rupture during pregnancy has been the driver for some surgeons to recommend immediate surgical resection.
Therefore, it is especially challenging when a large pancreatic SPN of the pancreas head is suspected in a pregnant woman, and its removal would require a pancreaticoduodenectomy. Here, we report our management of such a patient for whom safe resection was done postpartum.
CASE REPORT
A 39-year-old woman underwent a routine fetal ultrasound in the 18th week of pregnancy, and a large solid and cystic mass in the region of the pancreas was seen. Non-contrast magnetic resonance imaging (MRI) revealed an 11.2 cm × 10 cm solid and cystic mass in the head of the pancreas (Fig. 1a and b), which was felt to be consistent with an SPN. Monthly abdominal ultrasonography revealed no growth of the mass. The patient did not experience abdominal pain, nausea or vomiting. At 40 weeks and 2 days, the mother had an uncomplicated spontaneous vaginal delivery of a healthy baby boy.
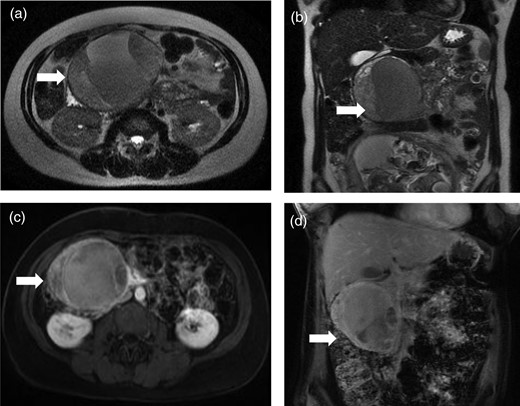
Magnetic resonance images reveal a well-circumscribed solid and cystic mass in the region of the pancreas head. Antepartum, non-contrast images in axial (a) and coronal (b) views. Postpartum, contrast-enhanced images in axial (c) and coronal (d) views.
Eight weeks after delivery, MRI with gadolinium showed a 9.3 cm × 6.8 cm solid and cystic mass in the head of the pancreas (Fig. 1c and d). There was no biliary or pancreatic duct dilatation. Major blood vessels appeared uninvolved.
Three months postpartum, she underwent a pylorus-preserving pancreaticoduodenectomy (Whipple procedure). The common bile duct and main pancreatic duct were not dilated, and the pancreas was soft. On gross pathology, a 10.6 cm × 7.5 cm encapsulated solid and cystic mass was seen arising from the pancreas head. The center of the mass appeared hemorrhagic and necrotic. The margins were negative, and 14 lymph nodes were free of tumor. By immunohistochemical analysis, positive staining for β-catenin, CD10, α1-antitrypsin, progesterone receptor and neuron-specific enolase was detected; chromogranin A expression was not observed. These morphologic and immunophenotypic features support the diagnosis of a pancreatic SPN [4].
She had an uncomplicated postoperative course and was discharged home on postoperative day 9 in good condition. Fourteen months after surgery, MRI with gadolinium did not detect any evidence of disease.
DISCUSSION
This case of a pregnant woman who is suspected of having an SPN in the head of the pancreas highlights several issues. First, serial imaging did not detect any growth of the pancreatic SPN over the remaining 22 weeks of pregnancy, and spontaneous rupture of the SPN did not occur despite observed expression of progesterone receptors on the patient's neoplasm and increased progesterone levels during pregnancy. The patient remained asymptomatic despite the growth of the gravid uterus. Second, a pancreaticoduodenectomy was successfully performed 3 months postpartum without any adverse consequences to the mother, and most importantly, to the fetus. At high-volume centers, mortality after pancreaticoduodenectomy is very low (<2%); however, morbidity remains high (∼40%) [5]. The safety—to the mother and fetus—of pancreaticoduodenectomy in a pregnant patient is largely unknown. This case demonstrates safe monitoring of tumor growth with ultrasound during pregnancy and uncomplicated pancreaticoduodenectomy after term delivery.
Third, when making imaging decisions during pregnancy, certain key points should be considered. Imaging procedures not associated with ionizing radiation are preferable and should be considered [6]. Ultrasonography and MRI are not associated with known adverse fetal effects. Intravenous gadolinium is contraindicated during pregnancy and should only be used if absolutely essential. Lactating women can breast feed without interruption after receiving iodinated contrast or gadolinium.
With close surveillance to monitor for tumor growth/rupture, safe resection was done postpartum for this pregnant patient diagnosed with an SPN and who remained asymptomatic.



