-
PDF
- Split View
-
Views
-
Cite
Cite
Man-Chi Lau, Peter Mhandu, Harry Parissis, Jim McGuigan, Primary diffuse B-cell lymphoma presenting as a solitary chest-wall lesion, Journal of Surgical Case Reports, Volume 2015, Issue 6, June 2015, rjv069, https://doi.org/10.1093/jscr/rjv069
Close - Share Icon Share
Abstract
Primary lymphoma presenting as a solitary lesion of the chest wall is extremely rare, as the majority of chest-wall tumours arise from metastasis. We demonstrate a case report of a 67-year-old male who underwent investigations for a chronic left-sided pleural effusion. A computed tomography scan demonstrated a large chest-wall lesion, without rib destruction. He subsequently underwent fine needle aspirations and excisional biopsy for a histological diagnosis.
INTRODUCTION
Diffuse large B-cell lymphoma (DLBCL) is the most common histological subtype of non-Hodgkin's lymphoma. However, presenting as a primary chest-wall lesion is a rare disease entity. The clinical symptoms are generally non-specific and can lead to a delay in diagnosis. Pretherapeutic evaluation usually includes a biopsy for histopathological diagnosis, and radiological imaging for subsequent staging. The mainstay of management is chemotherapy, as surgical resection remains a controversial role.
We demonstrate through a case report how DLBCL was diagnosed in this patient, following investigations for a chronic left-sided pleural effusion.
CASE REPORT
A 67-year-old gentleman was admitted to a District General Hospital under a respiratory team for investigations of a chronic left-sided pleural effusion. He had symptoms of malaise, poor appetite and weight loss. His past medical history included a myocardial infarction, asbestosis exposure, ex-smoker of 60 pack years, recurrent lower respiratory tract infections, atrial fibrillation, chronic kidney disease and osteoporosis.
Subsequent high-resolution computed tomography (CT) chest demonstrated a well-defined lesion of 7.4 cm × 7.6 cm of reduced attenuation in the left lateral chest wall, encasing seventh and eighth ribs, without rib destruction (Fig. 1).
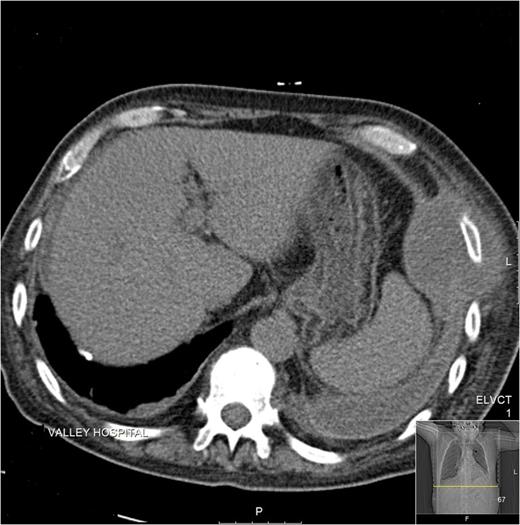
CT image demonstrating a well-defined chest-wall lesion encasing ribs, without rib destruction.
Two fine needle aspirates (FNA) failed to yield definitive histology, even though cytology assessment of pleural fluid was in keeping with malignancy; however, origin could not be identified.
The patient, therefore, was referred to the cardiothoracics team and underwent an excisional biopsy of the chest-wall lesion under local anaesthetic as he was not fit for a general anaesthetic. The histopathology results of this biopsy were suggestive of DLBCL, which was positive for CD30 but negative for Hodgkin's and anaplastic lymphomas. Epstein-Barr encoding region in situ hybridization strongly positive is suggestive of that it could be driven by Epstein Barr Virus (EBV). The patient had no history of this.
The patient underwent staging CT of the brain and the abdomen that demonstrated no evidence of metastasis. He was discussed at a Regional Haematology Multidisciplinary Meeting, which concluded that, given his comorbidities, it was felt that chemotherapy was not appropriate and the plan was for supportive palliative management. He received regular packed red cell transfusions but died ∼2 months after his definitive diagnosis.
DISCUSSION
Lymphoma presenting as a solitary chest-wall lesion is quite rare. Press et al. [1] found that only 4 out of 250 patients with lymphoma presented as isolated chest-wall disease. In reports of primary lymphoma of the chest wall, DLBCL is the most common subtype [2]. Most lymphomas do affect the thorax at some stage during the course of the disease; however, it is reported that <2% of chest-wall tumours are lymphomas [2–5].
DLBCL is an aggressive type of non-Hodgkin's lymphoma that affects the B-cells. The most common age of diagnosis is 60 years. It is slightly more common in men than in women. It constitutes about 30% of all non-Hodgkin's lymphomas [2]. Often, the first presentation is a rapid painless swelling in the neck, axilla or groin, which is caused by enlarged lymph nodes [3]. For some patients, the swelling may be painful. Other symptoms include night sweats, unexplained fevers and weight loss.
Most DLBCLs of the chest wall are frequently reported in the literature to be pyothorax-associated lymphomas [6]. They are also strongly associated with the latent form of the EBV. Cytokines produced at the site of chronic inflammation may induce a local immunosuppressive environment [6]. Another reported theory is trauma to the thorax. Our patient had no history of chronic pyothorax or chest-wall trauma. However, his strong smoking and occupational history may have contributed to the disease process.
Whilst findings of thoracic lymphoma may be evident on plain chest radiography, CT has traditionally been used to evaluate the disease and extent of spread. However, additional modalities such as magnetic resonance imaging (MRI) and positron emission tomography (PET)/CT have emerged. Thoracic MRI is useful in assessing vascular, cardiac and chest-wall involvement. PET/CT is more accurate in the overall staging of lymphoma than CT alone and can be used to evaluate treatment response [2].
Studies have suggested the importance of surgery in the role of the diagnosis of lymphomas. In this particular case, surgery was important as multiple fine needle aspirations had failed to yield a definitive diagnosis. In one study, the accuracy of diagnosis of lymphomas by FNA was exceptionally low. Some authors have suggested that patients with primary chest-wall malignancies should receive an excisional biopsy [7, 8]. FNA is frequently used as a first-line approach, but further procedures are often undertaken for definitive diagnosis and cell typing.
Chemotherapy is the main treatment for DLBCL, with or without chest-wall involvement. The most common regime is cyclophosphamide, doxorubicin, vincristine and prednisolone (CHOP). It remains controversial whether patients with lymphoma located only in the chest wall should undergo surgical resection. Ryan et al. [9] reported of a patient who underwent surgical resection for a primary chest-wall lymphoma had remained disease free for 4 years. Romagurea et al. [10] reported that surgical debulking is associated with improved survival in Stage I–II diffuse large-cell lymphoma. Hsu et al. reported a series of four patients who had isolated chest-wall lymphoma treated with surgical resection and adjuvant chemotherapy. Three of these patients remained disease free during their follow-up period.
CONFLICT OF INTEREST STATEMENT
None declared.



