-
PDF
- Split View
-
Views
-
Cite
Cite
Amad N. Khan, Salema Khalid, Mohammad Naushad Chaudhry, Cherrie Ho, Caecal perforation from TB and the Law of Laplace, Journal of Surgical Case Reports, Volume 2015, Issue 5, May 2015, rjv058, https://doi.org/10.1093/jscr/rjv058
Close - Share Icon Share
Abstract
A 43-year-old man presented to the hospital with haemoptysis. When worked up, his history and examination were highly suggestive of pulmonary tuberculosis (TB). He subsequently developed a massive upper gastrointestinal bleed and underwent an emergency laparotomy, which revealed a massively dilated caecum measuring ∼20 cm in diameter. The caecum had perforated due to acute decompensation of intestinal TB. Though common in developing countries, TB is rare in the UK, especially the intestinal kind. The most striking feature of this case is, however, the size of the caecal distension caused by the tubercular inflammation and subsequent perforation—something unheard of in the literature. This massive caecal distention would be explained by the Law of Laplace. In conclusion, massive distension and caecal perforation are possible consequences of intestinal TB, especially in the 48–72 h immediately after starting anti-tubercular therapy.
INTRODUCTION
According to estimates by the WHO, there are approximately 9.4 million patients a year diagnosed with tuberculosis (TB), with an annual mortality of 1.7 million [1]. Historically, the majority of TB cases are pulmonary; however, cases of extrapulmonary TB, including abdominal TB, are increasingly being reported in the UK [2]. Traditionally thought to be a disease of developing Asian and African countries, it is now increasing in prevalence in the West. Contributing factors to the rising incidence of abdominal TB in the UK are the increasing prevalence of HIV, immigration from developing countries and an ageing population [3, 4]. Abdominal TB often involves the gastrointestinal (GI) tract, peritoneum, mesentery, abdominal lymph nodes and solid organs, and usually causes non-specific symptoms like in our case, making the diagnosis difficult and a high index of suspicion necessary [5]. We, here, present the case of an immunocompetent patient, from a non-TB endemic country, who developed intestinal TB involving the caecum. A right hemicolectomy was performed and anti-tubercular treatment was initiated.
CASE REPORT
A 43-year-old Afro-Caribbean gentleman was admitted to the ED suffering from haemoptysis. He had previously been noted to have an enlarged lymph node in the right posterior triangle of neck which had been biopsied. At the time of presentation, the results of the histopathology were pending. He had also been suffering from weight loss of ∼18 kg over the previous 3 months along with night sweats and a reduced appetite. On examination, there was reduced air entry noted in the right lung on auscultation.
Since his history and clinical findings were very suspicious of TB, he was reviewed by the respiratory team. Empirical anti-tubercular therapy was suggested after sputum cultures were sent for acid fast bacilli (AFB) and a CT thorax showed a right upper lobe collapse and a 3-cm apicoposterior cavity. There was also consolidation seen in the right middle and lower zone as well as the left lung (Fig. 1). Also noted was right-sided neck lymphadenopathy (largest 17 mm). All these findings were consistent with pulmonary TB.

CT thorax—right-sided upper and mid zone collapse + consolidation.
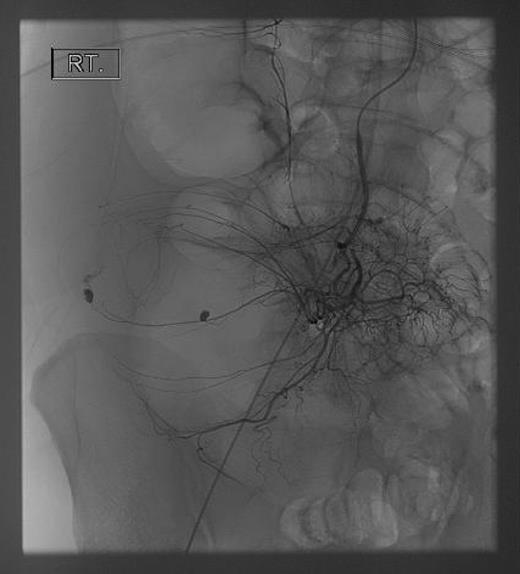
Seventy-two hours after starting his anti-tubercular therapy, he took a turn for the worse and was transferred to the ICU for ventilatory and inotropic support. He had ∼1 l of bleeding per rectum and dropped his haemoglobin (Hb) from 140 to 65 g/l. An oesophagogastroduodenoscopy showed no cause for upper GI bleeding. A CT abdomen + pelvis with contrast was performed, which showed a large (20 cm) inflammatory caecal mass with a moderate amount of intra-abdominal free fluid (Fig. 2). Selective angiography of the superior mesenteric artery demonstrated the bleeding point in the caecum and this was embolized superselectively with coils (Fig. 3).
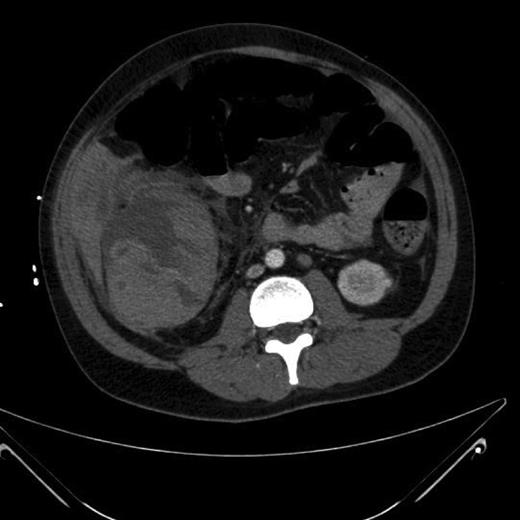
CT abdomen + pelvis with contrast: large inflammatory caecal mass.
His bleeding continues post-embolization, so a midline laparotomy was performed. The ascending colon was distended and very friable on mobilization. The posterior wall of the caecum was perforated and visibly the nidus of the bleeding (Fig. 4). The terminal ileum was normal and there was no gross lymphadenopathy. A right hemicolectomy was performed with primary stapled anastomosis.

Grossly enlarged and perforated caecum with a suction device demonstrating the depth of the cavity.
Postoperatively, the patient made a good recovery and had no further episodes of bleeding or drop in Hb. The histology from both the initial lymph node biopsy as well as the caecal mass came back positive for TB, as did his sputum cultures. He was discharged on post-op day 10 with a plan to complete his full course of anti-tubercular therapy and undergo both surgical and respiratory outpatient follow up.
DISCUSSION
GI involvement of TB can result in stricture formation, intestinal obstruction, perforation, fistulas and small bowel volvulus [6]. Intestinal perforation is uncommon but when does occur is a serious and life-threatening complication—mortality rates secondary to perforation are estimated to be >30% [7]. Early recognition of abdominal symptoms and intervention may improve the prognosis of tuberculous intestinal perforations. Recommended treatment is the resection of the affected bowel followed by end-to-end anastomosis [4]. However, for an inflammatory caecal mass of uncertain aetiology as in our case, right hemicolectomy has been recommended because of the concern of possible malignancy [8].
Some perforations occur before or shortly after antituberculous therapy begins [8], suggesting a natural progression of the condition, thought to be caused by a reactive thickening of the peritoneum and subsequent adhesion formations, leading to proximal dilatation and perforation [8]. Other cases had evidence of improvement during the course of treatment, before a later perforation. There have also been multiple cases of intestinal perforations occurring after completion of antituberculous therapy [8]. It has been hypothesized that a paradoxical response to treatment may be responsible for these cases [8]. This is similar to the disease progression in our case—the previously asymptomatic patient from the GI point of view acutely decompensated and developed caecal distention and perforation within 72 h stating anti-tubercular therapy.
Isolated caecal perforation that too tubercular in origin is extremely rare and only one other case has been reported [9]. If perforation does occur, it is in accordance with Laplace's law which states that the intraluminal pressure needed to stretch the wall of a hollow tube is inversely proportional to its radius [9]. The caecum has the largest diameter of the colon and therefore requires the least amount of pressure to distend [10]. Perforation of the caecum has been found to occur when the diameter reaches 16 cm—in our case, it was 20 cm and therefore perforation was not unexpected [10]. The extent of caecal distension seen in our case is unheard of in the literature and underlines the insidious nature of intestinal TB: our patient never complained of any GI signs or symptoms to suggest intestinal TB until he decompensated and bleed massively per rectum.
In conclusion, diagnosis of intestinal TB can be challenging hence requiring a high index of suspicion and caecal distension, and perforation can be paradoxically triggered by anti-tubercular therapy. Furthermore, the massive distension of the caecum reported in our case can be explained by Laplace's Law.
CONFLICT OF INTEREST STATEMENT
None declared.



