-
PDF
- Split View
-
Views
-
Cite
Cite
Tomotsugu Nakano, Yoshiaki Hara, Masamitsu Shirokawa, Sadaaki Shioiri, Hideaki Goto, Masamichi Yasuno, Michio Tanaka, Hemorrhagic giant cystic lymphangioma of the liver in an adult female, Journal of Surgical Case Reports, Volume 2015, Issue 4, April 2015, rjv033, https://doi.org/10.1093/jscr/rjv033
Close - Share Icon Share
Abstract
An 18-year-old woman who presented with epigastric pain was diagnosed with rupture of a hepatic tumor and transported to our hospital. Contrast-enhanced computed tomography revealed a 13-cm, low-density giant mass in the left hepatic lobe and high-density ascites, indicating abdominal bleeding from the liver tumor. The patient underwent emergent celiac angiography, and the left hepatic artery, which was believed to feed the tumor, was embolized. After the patient's condition stabilized, she underwent left hepatic lobectomy. In addition, the enlarged lymph nodes of the hepatoduodenal ligament were dissected. On microscopic examination, immunohistochemical staining revealed that both the liver cyst and the enlarged lymph node were positive for the endothelial marker CD31 and lymphangial marker D2-40. The patient was pathologically diagnosed with cystic lymphangioma of the liver. She has now been followed up for almost 4 years after surgery without any sign of recurrence.
INTRODUCTION
Among many types of benign hepatic tumors, hepatic lymphangiomas are rare congenital tumors most commonly observed among children and very rarely among adults [1]. Lymphangiomas are mostly found in the head and neck region and occur very rarely in the abdominal organs [2]. We describe a young female patient with huge cystic lymphangioma of the liver, which was manifested by hemorrhage and treated with surgical resection.
CASE REPORT
An 18-year-old woman presented with epigastric pain that started during a Japanese drum lesson. She was diagnosed with rupture of a hepatic tumor and transported to our hospital. She had no medical history of surgery, including abdominal surgery. Contrast-enhanced computed tomography (CT) revealed a 13-cm, low-density giant mass in the left hepatic lobe and high-density ascites, indicating abdominal bleeding from the liver tumor (Fig. 1). Ultrasonography confirmed a well-defined giant mass of the liver, comprising both cystic and solid lesions. Laboratory data showed a low hemoglobin level of 8.2 g/dl, and all the results of liver function tests and tumor marker measurement were within normal ranges. The patient underwent emergent celiac angiography, which revealed an avascular tumor with no evidence of extravasation from the hepatic artery. The left hepatic artery was considered to be the artery feeding the tumor and was embolized (Fig. 2). Magnetic resonance imaging (MRI) confirmed a well-defined giant multilocular lesion with fibrous partition (Fig. 3). After the patient's condition stabilized, she underwent left hepatic lobectomy. Laparotomy revealed bloody ascites and a large tumor in the left lobe of the liver; the right lobe appeared normal. The enlarged lymph nodes of the hepatoduodenal ligament were also dissected. Histological analysis of the resected specimen revealed a huge cystic mass of ∼12 × 9.5 cm. The mass was cystic and multilocular with a fibrous wall and filled with a massive blood clot (Fig. 4). The enlarged lymph node had a 25 × 23-mm cyst, which contained yellowish fluid. On microscopic examination, the wall of the cyst consisted of a tight elastic fiber meshwork composed of collagen fibers, which was accompanied by a small amount of acid mucopolysaccharide in the stroma and a lining of single-layered flat cells on the inner wall (Fig. 5a and b). Immunohistochemical staining revealed that the cyst wall was positive for both the endothelial marker CD31 and the lymphangial marker D2-40 (Fig. 5c and d). The cystic structure of the lymph node also was composed of elastic fiber components similar to those of the cyst in the liver and lined with single-layered flat cells, which were immunohistochemically positive both for CD31 and D2-40 (Fig. 5e). The pathological diagnosis was hepatic lymphangioma combined with lymphangioma of the lymph nodes. The patient's postoperative course was uneventful, and she was discharged on Day 8. During follow-up for almost 4 years since the surgical treatment, the patient has presented no sign of recurrence.
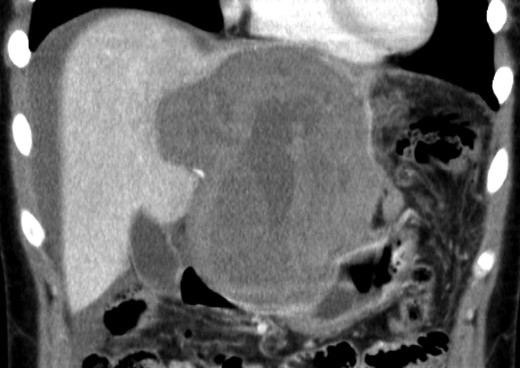
Enhanced CT scan demonstrated a low-density giant mass 13 cm in size and high-density ascites.
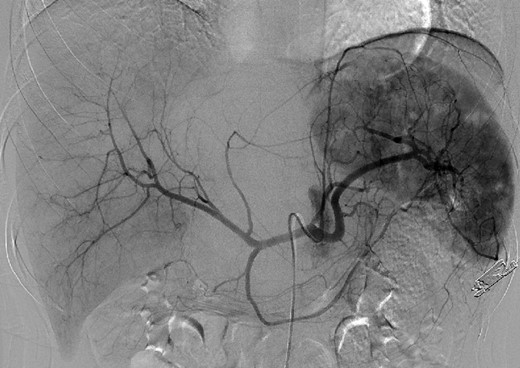
Emergent angiography demonstrated an avascular tumor and did not reveal any extravasation from the hepatic artery.
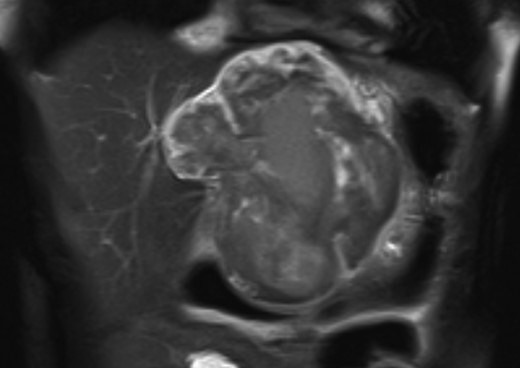
MRI confirmed a well-defined giant multilocular lesion with fibrous partitioning.
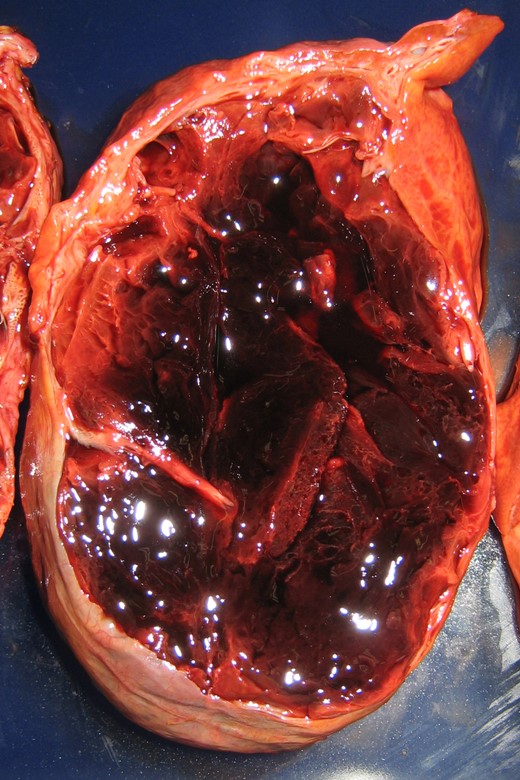
The mass was cystic and multilocular with a fibrous cystic wall and was macroscopically filled with a massive blood clot.
![(a) Multiple cystic spaces were lined with single-layered flat cells accompanied by papillary structures [hematoxylin and eosin (H&E) staining; magnification ×40]. (b) The cyst wall consisted of a tight elastic fiber meshwork containing collagen fibers (Elastica van Gieson staining; magnification ×40) (c and d) The wall of the liver cyst was positive for CD31 (magnification ×100) and D2-40 (magnification ×100) (e) The wall of the cyst in the enlarged lymph node was also positive for D2-40 (magnification ×100).](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2015/4/10.1093_jscr_rjv033/2/m_rjv03305.jpeg?Expires=1772272067&Signature=DQ-vQ-YSjbggWRSNc3rrw9USmHiylRM04quOLvBkNNfdh~dfCRkmKlXyRvpwsZMYwc6iqPx3TsaRoSawnhnp3TvmUs0AmfLYomeRcAe5QS05mEFHh13mWM~0wI9UOqOtSSdqndGJDJ6SKl56lDMmZmINfYnS4RcVY2lLTeiu3puWmc4X4HfB8r3OzBoC-dvfSGEq4oykegtpu70-2Yvi6ISf3bONU9bs2t9HBOGTwG0rI8ilYzPJd0ekBJw1CzeL9rLmmAuKZcGwCu39Avu2a-k6HuDd6U-xolqgh19iAOtwylNK-GGK2F0ReAcA8HIXSiV~px9Elo3pXfS6jp-E4g__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
(a) Multiple cystic spaces were lined with single-layered flat cells accompanied by papillary structures [hematoxylin and eosin (H&E) staining; magnification ×40]. (b) The cyst wall consisted of a tight elastic fiber meshwork containing collagen fibers (Elastica van Gieson staining; magnification ×40) (c and d) The wall of the liver cyst was positive for CD31 (magnification ×100) and D2-40 (magnification ×100) (e) The wall of the cyst in the enlarged lymph node was also positive for D2-40 (magnification ×100).
DISCUSSION
The etiology of lymphangioma remains unclear. Dysplasia of lymphatic tissue and abnormal development of lymph vessels are considered a possible mechanism for congenital malformation, and obstruction of lymphatic channels due to inflammation or trauma as another possibility for acquired abnormalities [1, 2]. Lymphangiomas are histologically classified into three main subtypes: cystic, capillary and cavernous [2]. Cystic lymphangiomas of the liver are very rare, and the first case was described by McQuown et al. in 1975 who reported the case of a benign cyst causing blockade of regional lymphatic flow [3]. Hepatic lymphangiomas are considered a subset of multiple abdominal lymphangiomas, and in most cases are accompanied by similar abnormality in other organs including the spleen, kidneys, lungs, mesentery, gastrointestinal tract and soft tissues [1]. In the present case, enlarged lymph nodes found in the hepatoduodenal ligament had similar cystic structures as those found in the liver, and these are considered to have developed because of the same disease.
Cystic lymphangiomas in the abdomen are usually asymptomatic. In the present case, the patient presented with pain in the entire abdominal region, which is considered to be a peritoneal sign of intraabdominal bleeding from the tumor. A hemorrhagic benign tumor of the liver is extremely rare. Although there are several reports of intracystic bleeding within liver cyst [4, 5], we were not able to find any report on bleeding from a cystic lymphangioma of the liver. The patient in our case presented with abdominal pain during a drum lesson, and thus there is a possibility that some external force to the abdomen may have caused intracystic bleeding, which led to intraabdominal hemorrhage.
Diagnosis of cystic lymphangioma is normally difficult, particularly in adults because CT/MRI findings are similar to those for other cystic tumors. With mesenchymal hamartoma, biliary cyst adenoma and cystadenocarcinoma also considered in the present case based on the CT/MRI findings, a precise diagnosis could only be achieved after surgery. In the present case, pathological diagnosis was also difficult, particularly for distinguishing cystic lymphangioma from cystic hemangioma. This was because blood was found not only in the cystic legion of the liver but also in those of the enlarged lymph nodes. Immunohistochemical staining revealed that both the cyst wall and enlarged lymph nodes were positive for the lymphatic endothelial marker D2-40 as well as the vascular endothelial marker CD31. D2-40 has been reported to be a highly specific antibody for the identification of lymphatic endothelium [6]. Furthermore, dilated lymph ducts were observed around the tumor, which also is consistent with the reported mechanism of lymphangioma. These findings supported the diagnosis of cystic lymphangioma of the liver and the lesional lymph nodes. In summary, this report presents the case of a young patient with hemorrhagic cystic lymphangioma of the liver accompanied by lymphangioma of the lesional lymph nodes, which occurred because of intracystic bleeding. Cystic lymphangioma should be considered as a differential diagnosis when patients present with a multiloculated cystic tumor in the liver. Complete resection remains a sufficiently safe and desirable treatment option for this type of benign liver tumor.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- angiogram
- ascites
- computed tomography
- hemorrhage
- immunohistochemistry
- celiac disease
- epigastric pain
- liver cyst
- liver neoplasms
- adult
- cd31 antigens
- endothelium
- lymphangioma, cystic
- rupture
- surgical procedures, operative
- abdomen
- liver
- neoplasms
- surgery specialty
- hepatectomy, total left lobectomy
- hepatoduodenal ligament
- left branch of hepatic artery
- liver lobe
- lymphadenopathy



