-
PDF
- Split View
-
Views
-
Cite
Cite
Shen Hwa Vun, Levent Bayam, Efstathios Drampalos, Mohammed Jesry, George Fadel, Floating patella associated with lymphoedema, Journal of Surgical Case Reports, Volume 2015, Issue 3, March 2015, rjv026, https://doi.org/10.1093/jscr/rjv026
Close - Share Icon Share
Abstract
Ipsilateral injury of more than one component of the knee extensor apparatus is rare. It is mostly associated with previous trauma, surgery, immunosuppression therapy and systemic disease. We present the first documented case of a spontaneous bifocal disruption of the knee extensor apparatus (i.e. floating patella) associated with lymphoedema. This case highlights the importance of considering lymphoedema as another risk factor for rupture of the knee extensor apparatus. It also highlights the importance of assessing all components of the knee extensor apparatus in patients presenting with acute knee injuries.
INTRODUCTION
Ipsilateral injury of more than one component of the knee extensor apparatus is rare and it is mostly associated with previous trauma, surgery, immunosuppression therapy and systemic disease. We report the first documented case of a spontaneous bifocal disruption of the knee extensor apparatus (i.e. floating patella) associated with lymphoedema in a 54-year-old man.
CASE REPORT
A 54-year-old man presented to our Accident and Emergency (A&E) department complaining of pain in his right knee. The patient has slipped off the bottom two steps of the staircase, without suffering any direct impact to his knee. He was still able to mobilize for 10 yards afterwards, before hearing a ‘pop’ and immediately experienced pain to his right knee.
There was no previous injury to patient's right knee. His past medical history included atrial fibrillation and squamous cell penile carcinoma of the glans penis, requiring partial penectomy and urethral reconstruction, and subsequent radical right inguinal lymph node (ILN) dissection 16 years ago (limited to borders of the femoral triangle) for lymphatic metastases, with clear dissections margins. Patient has never received any radiotherapy or chemotherapy treatment. He has been free from disease recurrence since, and continued to have annual surveillance follow-up. Following ILN dissection, patient developed right lower limb lymphoedema, with episodes of intermittent swelling of his right thigh, which became more frequent over the last 3 years. Patient was on warfarin, paracetamol and codeine. There was no family history of musculoskeletal, autoimmune disease, diabetes or other systemic disease.
Physical examination showed knee swelling, a high riding patella with a palpable gap below the patella. The patient was unable to weight bear and could not perform active knee extension on his right knee. There was no obvious laceration or injury to the knee. Neurovascular examination was normal. Apart from ectopic ossification of the patellar tendon, plain radiograph showed no evidence of acute fracture or joint effusion (Fig. 1). Because of the unusual mechanism of injury and the initial ultrasound performed in A&E which suggested a rupture of the quadriceps and patella tendon, magnetic resonance imaging (MRI) was performed and demonstrated complete rupture of the patellar tendon from the inferior pole of patella, an almost complete shearing of quadriceps tendon off the patella and chronic tendinosis in the mid-portion of patellar tendon (Fig. 2).

Lateral radiograph of right knee, demonstrating patella alta and ectopic ossification of the patellar tendon (marked *). No evidence of acute fracture.
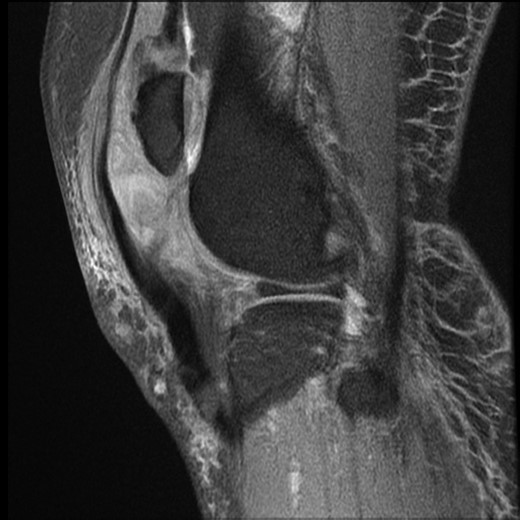
MRI right knee. Sagittal T1 image. Demonstrating rupture patellar tendon attachment from inferior pole of patella, high riding patella, chronic tendinosis of patellar tendon and clustering of sheared quadriceps tendon.
Surgery was performed on the knee. A midline longitudinal incision was made, revealing a complete rupture of the patellar tendon from the inferior pole of the patella, torn medial and lateral retinacular fibres, and near complete shearing of 90% of the quadriceps tendon (Fig. 3). The patellar tendon was anchored trans-osseously with 5 TiCron™ (Covidien) sutures, and further strengthened with 2/0 vicryl sutures using the Kessler technique. Both the quadriceps tendon and retinaculum were primarily repaired using 2/0 vicryl sutures. Postoperatively, the knee was immobilized in a long leg back slab for 2 weeks, followed by cylinder cast for 4 weeks. Patient was gradually worked towards full weight bearing afterwards. At 8 weeks post-surgery, patient was able to fully extend his knee, and perform straight leg raise against gravity. His range of flexion improved with physiotherapy from 30° to 100° at 3 months following surgery.
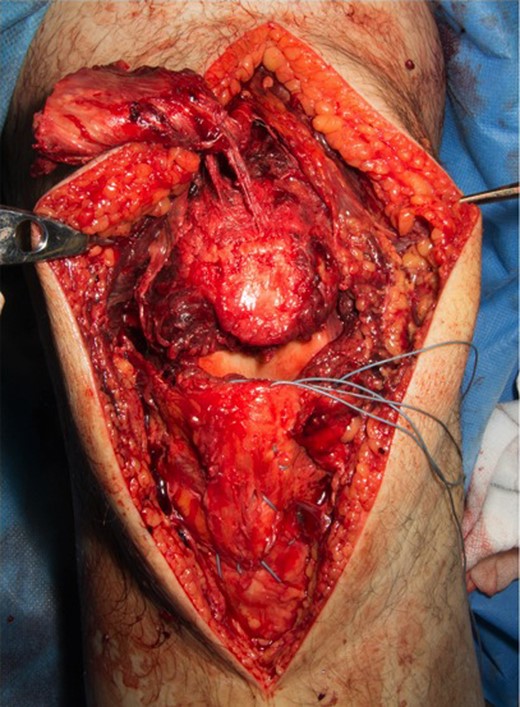
Intra-operative image demonstrating shearing of the quadriceps tendon, complete patellar tendon rupture, and injuries to medial and lateral retinaculum.
DISCUSSION
Injuries to more than one knee extensor apparatus are rarely encountered in the literature [1]. The term ‘bifocal injury’ was used in the literature to describe any two injury involving patella/patellar tendon/quadriceps tendon/avulsion of tibial tubercle [1]. Kang et al. [1] classified bifocal injuries into five types. With a ruptured patellar tendon and shearing of quadriceps tendon, our patient has sustained a type 5 bifocal injury.
Rupture of the knee extensor apparatus commonly affects pathological tendons— microtrauma in athletes, chronic corticosteroid intake, immunosuppressant therapy, prior knee surgery, and systemic disease such as renal failure, diabetes, hyperparathyroidism, systemic lupus erythematous, gout and obesity [2–5]. It is well known that radical ILN dissection for penile cancer metastases is associated with lymphoedema of the ipsilateral leg [6].
Although lymphoedema following breast surgery has been associated with rotator cuff tendonitis/tear [7]; so far, the association between lymphoedema and rupture of the knee extensor apparatus has not been documented in the literature. Herrera and Stubblefield [7] first described the pathophysiology of rotator cuff tendonitis secondary to lymphoedema following axillary clearance breast cancer surgery. They believed the increased size and weight on the upper limb caused by interstitial stagnation of protein-rich fluid lymphoedema subjects the rotator cuff tendons to impingement, functional overload and intrinsic tendinopathy. With vascular studies demonstrating the presence of a hypovascular zone in quadriceps tendon (1–2 cm from superior pole of patella) frequently associated with spontaneous rupture [8], and the MRI image in our patient showing chronic tendinosis of the patellar tendon (Fig. 2), it is most likely that chronic lymphoedema was the main aetiological factor in this spontaneous non-traumatic bifocal injury of the knee extensor apparatus. This is likely secondary to the resultant chronic inflammation and fibrosis from chronic lymphoedema, which compromised perfusion and tendon/connective tissue homeostasis, therefore predisposing the retinaculum, quadriceps and patellar tendon to a risk of rupture.
To the best of our knowledge, this is the first reported case of spontaneous quadriceps tendon, patellar tendon and retinaculum rupture in an adult with lymphoedema in the literature. Our case highlighted the importance of considering lymphoedema as another pathoaetiological risk factor of knee extensor apparatus rupture. It also highlighted the importance of assessing all components of the extensor apparatus in patients presenting with acute knee injuries. Spontaneous rupture of several components of the knee extensor apparatus can sometimes be overlooked and missed, which could lead to significant implications during operative management.
CONFLICT OF INTEREST
None declared.



