-
PDF
- Split View
-
Views
-
Cite
Cite
Karleigh R. Curfman, R. Jonathan Robitsek, David Sammett, Sebastian D. Schubl, Blunt trauma resulting in pneumothorax with progression to pneumoperitoneum: a unique diagnosis with predicament in management, Journal of Surgical Case Reports, Volume 2015, Issue 12, December 2015, rjv147, https://doi.org/10.1093/jscr/rjv147
Close - Share Icon Share
Abstract
Here, we present a case of pneumoperitoneum caused by traumatic pneumothorax after a fall. The patient is an 82-year-old male who was brought into the emergency department after being found at the bottom of a flight of stairs with a bleeding scalp laceration. Upon presentation, the patient underwent emergent intubation followed by tube thoracostomy placement, had necessary imaging and was transferred to the surgical intensive care unit (SICU). Imaging revealed signs of pneumomediastinum and pneumoperitoneum in addition to the partially resolved pneumothorax. In the SICU, the patient became hemodynamically unstable requiring vasopressor support, which in the face of documented pneumoperitoneum without a clear cause mandated exploration. He was taken to the operating room for suspected viscus perforation, though none was found after extensively searching during an exploratory laparotomy. We suspect the patient developed pneumomediastinum and pneumoperitoneum as a result of traumatic pneumothorax, hastened by his subsequent intubation and mechanical ventilation.
INTRODUCTION
Pneumoperitoneum, the presence of free air within the peritoneal cavity outside of the viscera, results from perforation of intra-abdominal organs in ∼90% of cases [1]. Approximately 5–15% of pneumoperitoneum cases are not due to intra-abdominal organ perforation but are the result of thoracic, gynecologic or other intra-abdominal pathologies [2]. Thoracic injuries leading to pneumomediastinum have several etiologies, arising predominantly from mechanical ventilation-induced barotrauma, but it can also occur after cardiopulmonary resuscitation, pneumothorax, tracheal rupture, median sternotomy and blast injury [2]. The flow of air from the thoracic cavity to the abdomen is a result of pressure differences, and intrathoracic pressures of 60 cm H2O or greater will result in subcutaneous emphysema and pneumoperitoneum from progression of air flow [3, 4].
Several cases of pneumoperitoneum have been reported following blunt trauma. In one report, patients were managed following blunt thoracoabdominal trauma over 17 years. Of 233 patients, 32 were positive for free air on radiograph; of which, 25 had a gastric perforation managed surgically. Another seven patients were without a hollow viscus intra-abdominal injury, though all had pneumothorax in common and the majority had other intra-abdominal injuries [5].
CASE REPORT
An 82-year-old male with past medical history of diabetes mellitus and alcohol abuse arrived by ambulance after being found unresponsive at the bottom of a flight of stairs with a scalp laceration. While en route to the hospital, two unsuccessful intubation attempts were made for a Glasgow coma scale (GCS) of 8. Upon arrival in the emergency department (ED), his GCS was determined to be 3 and was intubated with use of the Glidescope. Physical examination revealed decreased breath sounds on the left and crepitus over the left chest wall, suggestive of subcutaneous emphysema, and an immediate tube thoracostomy was performed prior to chest X-ray (CXR) to reduce the suspected pneumothorax. CXR post chest tube placement demonstrated large amounts of subcutaneous emphysema (Fig. 1 ), which was also visible on computed tomography (CT) scan along with evidence of pneumomediastinum and pneumoperitoneum (Fig. 2), with pneumoretroperitoneum and pneumoperitoneum present on abdominal CT scan (Fig. 3). As a result of the fall, he also sustained a fracture of the right frontal bone, fractures of the C2 and C3 vertebrae, and mild subarachnoid and subdural hemorrhage without shift. There were no intra-abdominal injuries found. He was admitted to the surgical intensive care unit (SICU) and maintained on mechanical ventilation, remaining hypotensive, hypothermic and mildly tachypneic, becoming increasingly unstable over the next 8 h. Due to the known pneumomediastinum, pneumoperitoneum and worsening instability, he was taken to the operating room for suspected viscus perforation and peritonitis. An exploratory laparotomy was performed, which revealed air within the lesser sac, but no evidence of bleeding or perforation. When closing the operative site, crepitus was also noted over the right chest wall, and a chest tube was placed into the right pleural space.
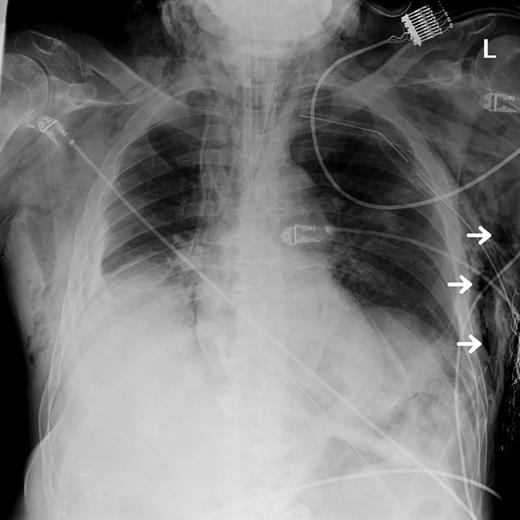
CXR performed after thoracostomy and chest tube placement displaying areas of subcutaneous emphysema (white arrows).

Chest CT scan obtained shortly after patient's arrival displaying evidence of subcutaneous emphysema (white arrow), pneumomediastinum (black arrow) and air tracking down resulting in pneumoperitoneum (gray arrow).
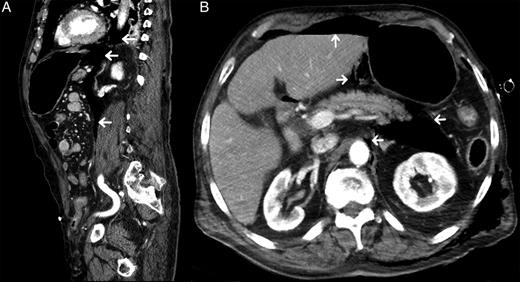
Sagittal view from CT abdomen/pelvis with contrast (A) showing areas of free air in mediastinum and thoracic cavity spreading downward into peritoneum (white arrows). Coronal view (B) showing free air within the abdominal cavity. Pockets are visible around the aorta, pancreas and liver (white arrows), as well as the presence of subcutaneous emphysema.
Postoperatively, the patient was rapidly weaned from all vasopressor agents, though he required persistent mechanical ventilation. He developed several complications including acute respiratory distress syndrome, pneumonia and acute renal failure with ongoing hyponatremia. He also developed several episodic seizures that were controlled medically. After 22 days in the SICU, the patient's family elected to pursue inpatient hospice care as the patient remained on mechanical ventilation and was generally non-responsive.
DISCUSSION
In our case, a fall caused a rib fracture that resulted in a lung laceration, leading to a pneumothorax. Subsequently, by virtue of the Macklin effect, the patient developed pneumomediastinum. The Macklin effect occurs when traumatic rupture of alveoli causes free air to travel along bronchovascular sheaths [3]. Intra-abdominal pressure is typically greater than intrathoracic pressure. However, in the setting of pneumothorax and pneumomediastinum, the intrathoracic pressure may be higher than intra-abdominal pressure. This pressure reversal forces free air from the thoracic cavity into the intra-abdominal cavity, resulting in pneumoperitoneum [4].
Two other reports describe pneumothorax progressing to pneumomediastinum and pneumoperitoneum after a fall [5, 6], whereas the majority of other reported cases were due to higher-energy traumas than our patient's fall [5, 7, 8]. Our patient had a tube thoracostomy performed on arrival in the ED, which should have released any accumulated intrathoracic pressure prior to developing pneumomediastinum and pneumoperitoneum. Other reported cases have theorized that delayed placement of the chest tube was responsible for the pneumoperitoneum, making this case unique in that regard.
Diagnosis of pneumoperitoneum is often only possible with imaging, initially on plain radiographs or by CT scans [9]. Patients with spontaneous pneumoperitoneum often undergo emergency laparotomy as a reflex response. Some have advanced the idea of nonsurgical treatment of spontaneous pneumoperitoneum in the absence of a pathological condition that necessitates surgical exploration. Hoover et al. produced an algorithm suggesting proper management of spontaneous pneumoperitoneum (Fig. 4), basing their primary recommendations for management on radiologic imaging, temperature, leukocyte count and physical examination [10]. Our patient was hypothermic, had a leukocyte count within normal limits and was unresponsive, so a proper abdominal examination could not be performed. Per this algorithm surgical exploration was not initially warranted and he should have been observed. However, our patient had worsening hypotension, tachycardia, hypothermia, tachypnea, acidosis with high anion gap and hypokalemia, and we felt it was pertinent to progress to laparotomy due to his decline in status. Though laparotomy did not reveal any perforations, the patient's vital signs normalized postoperatively over the next 24 h.
![Adaptation of the algorithm initially proposed by Hoover et al. [10] for managing spontaneous pneumoperitoneum.](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2015/12/10.1093_jscr_rjv147/2/m_rjv14704.jpeg?Expires=1772272032&Signature=Ylvpg5xmwpRBSD93H5uovCPiSJlEDayTZbdRbkpWk7rb7DtlPh0UM0nYYifPU4oJAn22tWltfcIdN7fHTZy-Br3nl4lk02JGP~BtgHqmLeJ370w4NcDZceR2SzXqkWNJwcvWd1HpKvTUppstGVBeAt2GqRQ7sjCSSL2~Il~GQjP2pfBxiYRGJ-ixgwjn0ZWz94mCb5GZQIhDtqq8pZxqtuneS2b8dIRsKaJtSCr0NhlPb2w0UFmpN24d8rNiFODyIpHziEf4t-wbe~TC4k5iLkKBgGMp2wRttBcd55TFTHl7NgxKgvzjOpf4Bh0dqKKTNtehrPRPwwXxDCRCrnEFyw__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
Adaptation of the algorithm initially proposed by Hoover et al. [10] for managing spontaneous pneumoperitoneum.
Pneumoperitoneum in the absence of hollow viscus perforation is uncommon, and even rarer when caused by low-impact traumatic pneumothorax without concomitant abdominal trauma. Similar cases have resulted from higher-impact trauma that allowed for the accumulation of greater intrathoracic pressures or delay in tube thoracostomy. The combination of low-impact trauma and immediate tube thoracostomy does not favor the development of pneumothorax progressing to pneumomediastinum and pneumoperitoneum, making this case unique. The development of subsequent hemodynamic instability has not previously been described, raising the possibility that even in the absence of intra-abdominal injury, releasing pneumoperitoneum via laparotomy may be beneficial. While surgical management is not necessary for all cases of pneumoperitoneum, due to our patient's worsening status, an exploratory laparotomy was warranted and was ultimately therapeutic.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- vasoconstrictor agents
- hemorrhage
- emergency service, hospital
- intubation
- mediastinal emphysema
- operating room
- nonpenetrating wounds
- diagnosis
- diagnostic imaging
- pneumoperitoneum
- pneumothorax
- viscera
- traumatic pneumothorax
- hemodynamic instability
- mechanical ventilation
- scalp laceration
- tube thoracostomy
- laparotomy, exploratory
- surgical intensive care unit
- endotracheal intubation, emergency procedure
- stairs



