-
PDF
- Split View
-
Views
-
Cite
Cite
Darren Leonard Scroggie, Maitham Al-Whouhayb, Asymptomatic giant appendicolith managed conservatively, Journal of Surgical Case Reports, Volume 2015, Issue 11, November 2015, rjv149, https://doi.org/10.1093/jscr/rjv149
Close - Share Icon Share
Abstract
A 67-year-old lady was found to have a giant appendicolith during a colorectal cancer screening colonoscopy, following a positive faecal occult blood test. Computed tomography confirmed the presence of a calcified giant appendicolith within the base of the appendix, which otherwise appeared normal. Appendicoliths are widely believed to be a major cause of acute appendicitis via obstruction of the appendix lumen, although this is disputed due to a lack of strong evidence. They may also cause chronic abdominal pain. All of the few cases of giant appendicoliths reported so far have been managed by extracting the lesions. Our patient was asymptomatic and had bilateral lung transplants, so a conservative watchful waiting approach was adopted. The authors propose expectant management of giant appendicoliths as a reasonable option in patients with significant operative risks.
INTRODUCTION
Appendicoliths are accumulations of faecal matter within and originating from the vermiform appendix, which may have a laminar structure and often become calcified [1]. They are recognized as a classical cause of acute appendicitis and have been implicated as a cause of chronic abdominal pain. A recent retrospective observational study of 254 patients, having undergone contrast-enhanced computed tomography (CT) followed by appendicectomy, identified the presence of appendicoliths in 46% [2]. They are usually <1 cm in their largest dimension; those >2 cm are termed giant appendicoliths. In cases of acute appendicitis, the presence of appendicoliths appears to be associated with more severe disease [2]. All reported cases of giant appendicoliths have been managed by extraction, either surgically or endoscopically, mostly due to the presence or perceived risk of appendicitis [3–7]. No data exist on the outcome of watchful waiting as a management strategy for asymptomatic giant appendicoliths. The massive size of such lesions implies chronicity without consequence, so conservative management may be an option in selected patients. The authors report a case of an asymptomatic giant appendicolith managed conservatively.
CASE REPORT
A 67-year-old lady had a positive faecal occult blood test, undertaken on the NHS Bowel Cancer Screening Programme. She had no gastrointestinal symptoms, and clinical examination of the abdomen was unremarkable. Her medical history included bilateral lung transplants for chronic obstructive pulmonary disease, Nissen fundoplication for gastro-oesophageal reflux disease, hypercholesterolaemia and macrocytic anaemia.
She subsequently had a colonoscopy, which revealed mild sigmoid diverticulosis and no mass lesions. The caecum appeared distorted by a large faecolith impacted in the appendiceal orifice. This was visible as an ovoid calcified lesion projected over the right sacral ala on a radiograph (Fig. 1) of the pelvis. A computed tomogram (Fig. 2) of the abdomen and pelvis demonstrated a giant calcified appendicolith, measuring 2.5 cm in its largest dimension, within the base of an otherwise normal appendix. Uncomplicated sigmoid diverticulosis was also noted.
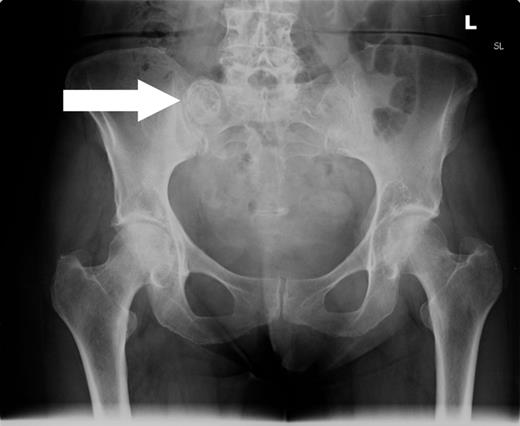
Anterior–posterior radiograph of the pelvis demonstrating a calcified ovoid lesion projected over the right sacral ala.

Axial, coronal and sagittal CT views showing a giant appendicolith within the base of the appendix. Calcification and the laminar structure are well demonstrated on CT.
The initial management was a watch-and-wait approach, due to the operative risks associated with her bilateral lung transplants. No further investigations were performed. She was advised to attend the emergency department immediately if she developed symptoms of acute appendicitis, which were explained to her. She was reviewed at 6-monthly intervals in the outpatient clinic and remained asymptomatic 1 year after the giant appendicolith was first detected endoscopically.
DISCUSSION
Appendicoliths have long been implicated in the pathogenesis of acute appendicitis, by initiating a sequence of events beginning with obstruction of the appendiceal lumen promoting subsequent bacterial invasion. However, little good quality evidence exists to support this widely held belief; thus, the role of obstruction as an early event is disputed [8]. Appendicoliths may also cause chronic or intermittent abdominal pain without appendicitis.
Those >2 cm are described as giant and are uncommon. Larger appendicoliths may be associated with more severe appendicitis [2]. There are relatively few reports of giant appendicoliths [1, 3–7]. The largest recorded was 3.5 cm [6]. The majority of patients were symptomatic; reported manifestations include acute appendicitis, chronic or intermittent abdominal pain and bleeding per rectum. Removal of the lesions has historically been the treatment of choice [1]. Laparotomy has been the most common approach, but two cases of endoscopic extraction have been described in recent years [3, 6]. Interestingly, both patients treated endoscopically had a history of previous appendicectomy, but were found to have a residual appendix stump containing the giant appendicolith. A causal relationship between the presence of a giant appendicolith and incomplete resection of the appendix cannot be concluded, but it is conceivable that a surgeon performing an appendicectomy might misidentify the base of the appendix in the presence of a giant appendicolith.
Our case is the first reported to be managed conservatively. The decision to adopt this approach was reached by mutual agreement of the patient and the multidisciplinary team. The principal factors influencing this decision were that the patient was asymptomatic, and that she had bilateral lung transplants. It was recognized that the presence of the giant appendicolith may have induced appendicitis in the future, necessitating emergency appendicectomy. It was not possible to objectively quantify this risk since there was no published data regarding the outcomes of asymptomatic giant appendicoliths managed conservatively. The patient was advised to attend the emergency department immediately if she experienced abdominal pain; this approach would have minimized diagnostic delay if she were to have developed appendicitis. Regular outpatient clinic follow-up appointments were planned to screen for more subtle symptoms.
Our case suggests that conservative management is a reasonable option when the patient is asymptomatic and has significant risks for operative management. It remains to be seen whether or not this patient will eventually require surgical intervention in the longer term.
CONFLICT OF INTEREST STATEMENT
None declared.



