-
PDF
- Split View
-
Views
-
Cite
Cite
A.Z. Nghiem, J.R. Wormald, S. Rodríguez Villar, An interesting case of an aortopulmonary artery fistula, Journal of Surgical Case Reports, Volume 2014, Issue 9, September 2014, rju079, https://doi.org/10.1093/jscr/rju079
Close - Share Icon Share
Abstract
Aortopulmonary artery fistulae are exceeding rare and may be associated with aortic arch aneurysms or thoracic aortic surgery. Here, we present a case of an aortopulmonary artery fistula in an 87-year-old woman with no history of aneursymal disease or thoracic surgery and discuss the likely aetiology and management of this condition.
INTRODUCTION
An aortopulmonary artery fistula is an exceptionally rare and often highly lethal condition, usually diagnosed on post-mortem. In these cases, it has been attributed to iatrogenic complications of thoracic aortic surgery, ruptured aortic arch aneurysms and also chronic infectious processes of the aorta or lung [1]. Here, we present a case of an 87-year-old woman with no history of an aortic aneurysm or previous aortic surgery presenting acutely with an aortopulmonary artery fistula.
CASE REPORT
An 87-year-old woman normally fit and independent with a history of well-controlled hypertension but no history of ischaemic heart disease presented overnight to the Emergency Department at a London District General Hospital complaining of acute onset central chest pain. The pain had developed suddenly during the afternoon and was associated thoracic back pain. A systolic blood pressure of 70 mm/Hg was recorded by her daughter at home, which together with her symptoms prompted a call to the emergency services.
On arrival to hospital she was fully alert and conversant despite her blood pressure was 75/35 mmHg with a heart rate of 120 b.p.m. Auscultation of the chest was unremarkable, an abdominal aortic aneurysm was not palpated, peripheral pulses were intact and there was no bilateral blood pressure difference.
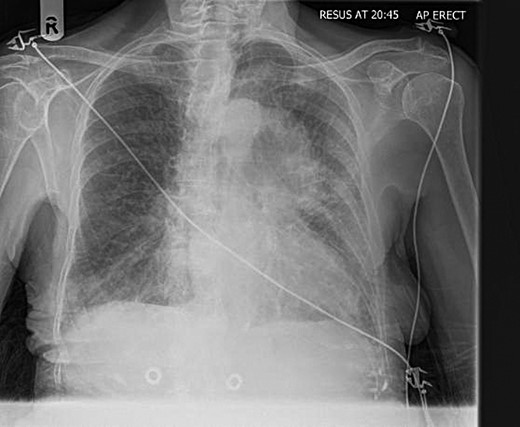
Her electrocardiogram showed ST segment depression in the lateral leads suggesting myocardial ischaemia. Her chest radiograph showed a well-circumscribed opacity appearing to arise to the left of the aortic arch (Fig. 1). Blood tests revealed haemoglobin of 13 g/dl.
During her chest radiograph the patient suddenly became unresponsive and even more hypotensive. She was intubated and ventilated in the emergency department and started on inotropic support. A computed tomography angiography (CTA) was performed for a suspected dissecting thoracic aorta before transfer to the intensive care unit.
The CTA showed a large 7.3 × 6.8 cm haematoma in the left anterior mediastinum with active contrast extravasation from the left main pulmonary artery (Fig. 2). There was a moderate left-sided effusion but no aortic aneurysm or dissection seen.

CT chest showing a mediastinal haematoma with active contrast extravasation.
An echocardiogram showed a large, non-echogenic mass external to the pericardium which was visibly compressing the left atrium.
The images were reviewed by the tertiary cardiothoracic and vascular surgery centres with regards to open surgical, hybrid or endovascular options. Unfortunately, the patient had deteriorated further and after a multidisciplinary discussion and discussion with the patient's family it was decided aggressive intervention would not be in the patient's best interest and in her current health would likely be futile. The patient died shortly after on the intensive care unit.
On post-mortem no evidence of aortic root dissection or cardiac hypertrophy was found. Immediately distal to the arch of the aorta there were two small defects in the aortic wall freely communicating with thrombotic material measuring 6 × 5 × 6 cm which communicated with an intimal tear of the left main pulmonary artery through a 1.5 cm defect. This fistula tract was concluded to have formed acutely.
DISCUSSION
Aortopulmonary artery fistulae are exquisitely rare. They may arise from chronic thoracic aortic aneurysms due to atherosclerosis or connective tissue disorders. Other pathology includes infection such as syphilis or inflammation seen in autoimmune vasculitides. More recently cases are related to surgical or endovascular procedures of the thoracic aorta [1].
In this case, there was no history of any aneurysmal disease, chronic infectious or inflammatory conditions or thoracic surgery. Given the sudden onset of symptoms, the most likely differential diagnosis clinically is an aortic dissection; however, the CTA and post-mortem excludes this. Based on the clinically picture, the findings on the chest radiograph, CTA and post-mortem we postulate alternative theories.
The mediastinal mass seen on plain chest radiograph and CTA may have represented a saccular aneurysm, which acutely ruptured into the pulmonary artery resulting in circulatory collapse. Another differential would be a neoplastic or infective mediastinal mass, which had invaded into the left main pulmonary artery over time creating a pseudo-aneurysm, which would not cause any clinically significant haemodynamic disturbances. This pseudo-aneurym increased in size over time and has ruptured into the thoracic aorta, which acutely presented with chest pain and circulatory collapse.
Early detection and subsequent management of such a mediastinal mass would have likely precluded this event. Presenting symptoms would have likely included a change in voice due to left recurrent laryngeal nerve involvement or raised left hemi diaphragm from left phrenic nerve involvement.
If the presentation of the aortopulmonary artery fistula was chronic, we would expect to see signs and symptoms of pulmonary hypertension and congestive heart failure [2]. On diagnosis, depending on the anatomy concerning the fistula a variety of procedures may be discussed, such as hybrid, arch reconstruction or endovascular stenting. This would be carefully planned and managed between the cardiothoracic and vascular surgeons as well as interventional radiologists [3–7].
Management in an acute setting is inherently more challenging due to often rapid clinical deterioration, difficulty in diagnosis and access to the relevant specialists. A high index of suspicion for thoracic aortic involvement is needed and this should be investigated with a CTA and an echocardiogram [8]. Early recognition and involvement of vascular and cardiothoracic teams is needed.
We report an exceedingly rare phenomenon of an aortopulmonary artery fistula with no history of aortic aneurysm or past surgery. We postulate this was due to a neoplastic or inflammatory process initially invading or involving the left main pulmonary artery and leading to the terminal event by rupturing into the thoracic aorta. This case highlights the difficulty in the diagnosis of this condition as well as the acute management of the condition.



