-
PDF
- Split View
-
Views
-
Cite
Cite
Tetsuya So, Reiko Mitsueda, Takeaki Miyata, Atsushi Sekimura, Takashi Yoshimatsu, Naohiro Nose, Hiroshi Itoh, Shigeo Nakano, Kosei Yasumoto, Pulmonary dirofilariasis in a 59-year-old man, Journal of Surgical Case Reports, Volume 2014, Issue 8, August 2014, rju082, https://doi.org/10.1093/jscr/rju082
Close - Share Icon Share
Abstract
We present a case of a human pulmonary dirofilariasis in a 59-year-old man. At the medical examination, a chest computed tomography (CT) revealed a mass, measuring 18 × 15 mm in diameter, with an irregular margin on the bottom of the right lower lobe. We could not neglect the possibility of a primary lung cancer, and therefore, a lung partial resection was performed under video-assisted thoracoscopic surgery. The intra-operative pathological findings revealed inflammatory granuloma with coagulation necrosis and no malignant cells. The permanent pathological examination showed occlusion of the peripheral pulmonary artery by worms and formation of a necrotic mass surrounded by reactive inflammation and hemorrhage. Human pulmonary dirofilariasis is an extremely rare zoonotic infection, and sometimes it is difficult to distinguish it from a primary lung cancer on radiographic findings.
INTRODUCTION
Human pulmonary dirofilariasis is a rare zoonotic infection caused by the dog heartworm Dirofilaria immitis, which is transmitted via a vector/intermediate host, generally the mosquito [1, 2]. Owing to the increase in the number of a medical examination, this disease has sometimes been reported recently. We herein report the rare case of a human pulmonary dirofilariasis.
CASE REPORT
A 59-year-old Japanese man visited our hospital in April 2013 for a workplace medical examination. He was a former smoker (from 20 to 26-year-old, 1 pack per day), and had neither physical symptoms nor family history of malignancies. The chest X-ray did not detect an abnormal shadow, but a CT showed a mass with an irregular margin measuring 18 × 15 mm in diameter at the subpleural area of S9 of the right lower lobe (Fig. 1). The CT detected no nodules in the other lobes or regional lymph nodes swelling. A FDG-PET was performed, but did not yield a definitive FDG accumulation (data not shown). Such tumor markers as CEA, SLX, SCC, CYFRA, NSE, and ProGRP were all within their normal ranges. In May 2013, a lung partial resection was performed under video-assisted thoracic surgery (VATS). At the time of thoracotomy, the mass located at the periphery of S9 of the right lower lobe and the surface was whitely transparent (Fig. 2A). The mass was solid and hard on palpation (Fig. 2B). The intra-operative pathological findings (frozen section) revealed inflammatory granuloma with coagulation necrosis. The permanent pathological examination showed occlusion of the peripheral pulmonary artery by worms and formation of a necrotic mass surrounded by reactive inflammatory cells and hemorrhage in hematoxylin–eosin stain (Fig. 3A) and Elastica van Gieson stain (Fig. 3B). Post-operative course was uneventful, and he is doing well 15 months after surgery.
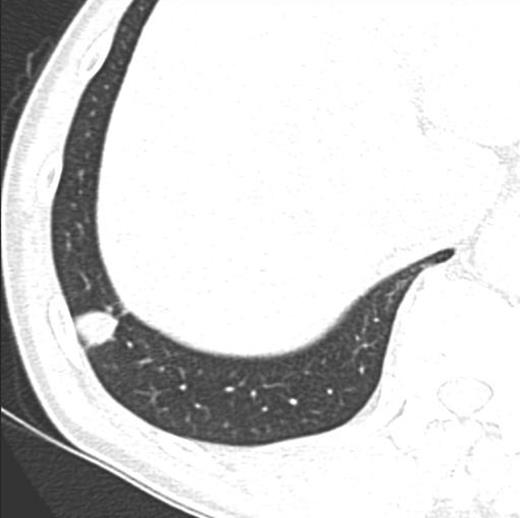
Pre-operative chest CT scan demonstrated the mass measuring 18 × 15 mm with spiculation at the periphery of S9 of the right lower lobe.
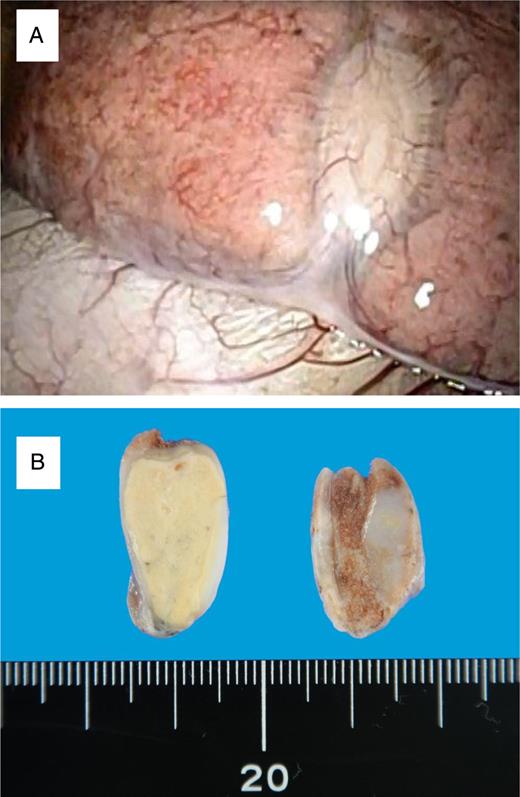
(A) Intra-operative thoracoscopy showed the white tumor with pleural indentation. (B) Macroscopic examination revealed white and solid tumor.
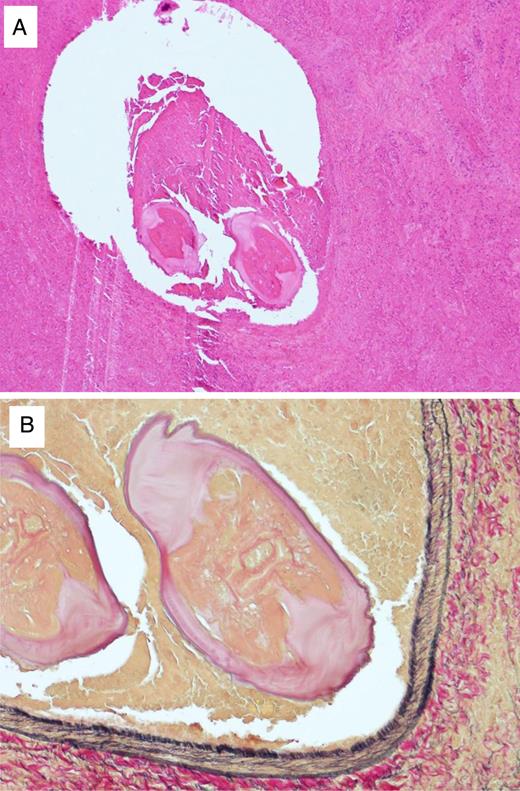
(A) Histopathological findings of the pulmonary nodule. Two transverse sections of an immature worm were seen in the peripheral pulmonary with fibrous tissue, necrotic tissue, and granulation (hematoxylin and eosin staining, ×6). (B) The transverse section in the peripheral pulmonary revealed layers of cuticle, internal longitudinal cuticular ridges and lateral chords, being identified as Dirofilaria immitis (Elastica van Gieson stain, ×20).
DISCUSSION
Human pulmonary dirofilariasis is a rare zoonotic infection caused by the canine heartworm Dirofilaria immitis [1, 2]. According to the medical database, De Magelhaes first described the discovery of filarial worm in the left ventricle of a Brazilian boy in 1887 [3]. Flieder and Moran [4] investigated that there were 31 of 41 nodules in the right side of the lung, and especially 19 of 31 nodules in the right lower lobe. In our case, he was asymptomatic and the mass was located in the right lower lobe. Furthermore, he bred a dog ∼20 years ago in our case. Milanez et al. [5] mentioned that the filarial infection rates of dogs were more important than the history of dog breeding.
The radiographic images of human pulmonary dirofilariasis have some specific features. It has been reported that the chest X-ray showed a solitary, round nodule in a lung field in many cases. In our case, however, the chest X-ray did not reveal the mass because of overlapping of the diaphragm. A chest CT can detect the disease as a mass measuring 18 × 15 mm in diameter at the periphery of the right lower lobe close to the lateral pleura. Recently, a FDG-PET has been applying for the qualitative diagnosis of lung nodules. The FDG-PET had been described in three cases of human pulmonary dirofilariasis for the differential diagnosis of pulmonary nodule [6]. The standardized uptake value (SUV) of them was reported from negative to 7.5, and the SUV was 1.4 in our case. In this way, the FDG-PET cannot deny a primary lung cancer pre-operatively.
Human pulmonary dirofilariasis is usually diagnosed by the surgical specimens, and it seems to be difficult to diagnose this disease by using the other modalities. For example, a filarial infection in human causes eosinophilia in general. Yoshimura et al. mentioned that human pulmonary dirofilariasis had little specific findings in hematological analysis and the average of eosinocytes in the peripheral blood was 6.5% [7]. In our case, the eosinocytes in the peripheral blood was 1.3 and 1.9% pre-operatively. The other examination to detect dirofilaria-specific antibody, such as an enzyme-linked immunosorbent assay, immunological electrophoresis and agglutination of red blood cells, has been reported to be useful [1, 7–9]. These immuno-serological analyses, however, have some problem as cross-reactivity and non-specificity between Dirofilaria immitis and the other filariasis. As a treatment, a lung resection has been performed which leads to final diagnosis and cure. Recently, a VATS seems to be a mainstream, and the benefit is less invasive for the patient [6, 10].
In conclusion, human pulmonary dirofilariasis is an extremely rare zoonotic infection, and sometimes mimick a primary lung cancer on radiographic findings. We, however, should be able to list up the one of differential diagnosis of lung cancer.
ACKNOWLEDGEMENTS
We thank Dr Tamotsu Kanazawa of University of Environmental and Occupational Health, Japan, for critical comments.



