-
PDF
- Split View
-
Views
-
Cite
Cite
Michaela Ramser, Anna Sarah Messmer, Isabella Zbinden, Urs Von Holzen, Christian Andreas Nebiker, Incarcerated obturator hernia–laparoscopic repair with intraoperative view of the corona mortis, Journal of Surgical Case Reports, Volume 2014, Issue 8, August 2014, rju081, https://doi.org/10.1093/jscr/rju081
Close - Share Icon Share
Abstract
Obturator hernias are a rare form of abdominal wall hernias. We present a case of a patient with an obturator hernia diagnosed by the classical signs of lower abdominal pain, a positive Howship–Romberg sign (painful internal rotation of the hip) and a computed tomography scan showing a herniated loop of small bowel. During the emergency laparoscopic hernia repair (transabdominal preperitoneal approach) a variant vessel, the corona mortis, was detected.
INTRODUCTION
Compared with the more common inguinal and femoral hernias, obturator hernias are rare with an incidence of 0.05–1.4% of all abdominal wall hernias [1]. Probably due to a wider pelvis and a more triangular obturator canal with a greater transverse diameter as well as previous history of pregnancy, obturator hernias are more common in elderly, emancipated women [2]. Since obturator hernias often become only clinically apparent when incarcerated, signs of acute small bowel obstruction can be found in 90% of patients with newly diagnosed obturator hernia. Owing to unspecific clinical signs and therefore often delayed diagnosis, advanced age of the patient, comorbidities and associated chronic disease mortality has been described as high as 47% [2–4].
CASE REPORT
A 97-year-old woman presented to the emergency department (ED) with a sudden onset of pain in the right lower abdomen with radiation to the right thigh. In her past medical history, the patient had bilateral open inguinal hernia repair and an open appendectomy.
The abdomen was tender with high-pitched bowel sounds in the right abdomen. No inguinal or femoral hernia was palpable, but coughing and internal rotation of her right hip caused increasing pain (Howship–Romberg sign).
Computed tomography (CT) scan revealed an obturator hernia on the right side with a herniated small bowel loop with early signs of incarceration (Fig. 1).

We performed an emergency laparoscopic transabdominal preperitoneal plasty (TAPP) to repair the hernia. During laparoscopy no herniated small bowel was present, but an erythema of a small bowel loop was seen not justifying a resection. The peritoneum forming the hernia sac was mobilized and opened. The hernia orifice could be displayed as shown in Fig. 2.
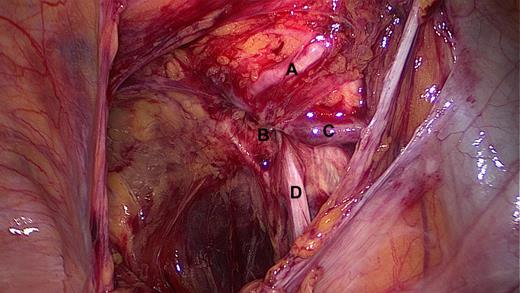
Intra-operative view after opening the peritoneum, showing the corona mortis (A) just above the obturator hernia orifice (B), the obturator vein with underneath the obturator artery (C) and the obturator nerve (D).
Apart from the obturator nerve and vessels, we detected a vessel crossing the pubic bone: the corona mortis (Fig. 2A). This vessel was spared from extra manipulation and the hernia closed with a monocryl-prolene mesh that was fixed with titanium tacks.
The post-operative course was uneventful. The patient left the hospital on the 13th post-operative day.
DISCUSSION
Obturator hernia is a rare form of abdominal wall hernia published the first time by de Ronsil in 1724. A compression of the obturator nerve by the hernia can cause pain or cramps from the groin to the knee. The symptoms can be even enforced by adduction and internal rotation of the thigh, which is called the Howship–Romberg sign.
In addition, compression of the obturator nerve can lead to an absent adductor reflex in the presence of a positive patellar reflex (Hannington–Kiff sign).
Pain from the groin to the knee might get mistaken for neuromuscular pain, as joint pain is common in elderly patients. Quite often diagnosis is missed and patient undergoes surgery for bowl obstruction and obturator hernia is diagnosed during the operation. If suspected preoperatively, the diagnostic modality of choice is nowadays the CT scan of the abdomen [3].
For the treatment of an obturator hernia, open and laparoscopic approaches have been described [5, 6]. The advantages of laparoscopic versus open abdominal surgery, namely less post-operative pain, earlier oral intake, shorter hospitalization, fewer risk of an incisional hernia and smaller wounds are well known. Furthermore, with the technical progress in laparoscopic surgery, transabdominal and extraperitoneal approaches are possible and have been described to be successful in obturator hernia repair [7, 8]. In our case, the transabdominal (TAPP) approach was chosen because of clinical and radiographic signs of incarceration. By the transabdominal approach a good visualization and assessment of the concerning bowel loop is possible.
As demonstrated by the positive clinical course, our patient with 97 years of age has been benefiting from the minimal invasive procedure.
Apart from the obturator hernia, a corona mortis, was visible during laparoscopy. The vessel is a variant connecting the inferior epigastric and the obturator artery. This so-called ‘crown of death’ has an incidence of up to 40% [9]. As an increasing number of abdominal hernias are repaired by a laparoscopic approach, surgeons should be aware of its existence and spare the vessel as severe bleedings can occur [10].
In summary, obturator hernias are rare and often present to the ED when incarcerated. Especially in elderly, thin women presenting with bowel obstruction and hip pain this exclusive type of hernia should be taken into consideration.



