-
PDF
- Split View
-
Views
-
Cite
Cite
Aiman Alassar, Adrian Marchbank, Left lower lobe torsion following upper lobectomy-prompt recognition and treatment improve survival, Journal of Surgical Case Reports, Volume 2014, Issue 8, August 2014, rju078, https://doi.org/10.1093/jscr/rju078
Close - Share Icon Share
Abstract
Lobar torsion is a rare but life-threatening complication after lung resection. We report a case of left lower lobe torsion in 57-year-old women after upper lobectomy for underlying lung cancer. Definitive diagnosis of lung torsion was made at exploratory thoracotomy following abnormal chest radiography and bronchoscopy on the first post-operative day. An emergency completion pneumonectomy was performed and left lower lobe was resected. The post-operative course was uncomplicated and patient was discharged home on the seventh post-operative day. Early recognition and prompt treatment of lobar torsion is essential for preventing potentially catastrophic complications including fatal gangrene of the pulmonary lobe.
CASE REPORT
A 57-year-old woman with a left upper lobe mass was referred to our institution for lung resection. Preoperative computed tomography (CT) and positron emission tomography were consistent with lung cancer. Pulmonary function tests revealed a forced expiratory volume in 1 s of 1.64 l (64% predicted), forced vital capacity of 3.1 l (104% predicted) and TLCO of 97% predicted. The patient underwent an uncomplicated left upper lobectomy through open thoracotomy. The fissures were complete, and the inferior pulmonary ligament was mobilized in part. A systematic nodal dissection was performed. She was extubated immediately after surgery and was transferred to the ward as per routine practice. Post-operative chest radiograph revealed satisfactory expansion of the left lower lobe (Fig. 1). On the first operative day, the patient remained haemodynamically stable, without systemic upset, but developed atrial fibrillation with tachycardia. Chest X-ray demonstrated complete opacification of the left hemithorax with normal position of the left hemidiaphragm (Fig. 2). Urgent rigid bronchoscopy revealed narrowed left lower lobe bronchial orifice and the bronchoscope could not pass through. The left upper lobe bronchial stump was intact. Immediate exploratory thoracotomy was performed. At surgery, the left lower lobe had undergone a 180° anti-clockwise torsion at its brochovascular pedicle. The lung parenchyma was very fragile and haemorrhagic, compatible with early venous infarction, hard with a dark reddish surface. Torsion of the lower lobe was corrected and lower lobe was sutured to pericardium, in order to further investigate the anatomy, and determine whether completion pneumonectomy could be avoided. Her AF resolved with restitution of the lobe. A minitracheostomy was inserted prophylactically. However, over the course of the first few post-operative hours, the patient became progressively more hypoxic and tachypnoeic. CT was performed, demonstrating acute obstruction with possible angulation of main pulmonary artery and complete obstruction of left main bronchus (Fig. 3), reported as demonstrating recurrent torsion. The patient returned to theatre for a third time, and at throacotomy, the lobe was found to be in its normal position, but there was now further evidence of infarction, and completion pnuemonectomy was performed. Histological examination confirmed haemorrhagic congestion throughout the left lower lobe parenchyma. Post-operative course was uneventful and patient was discharged home on Day 7.
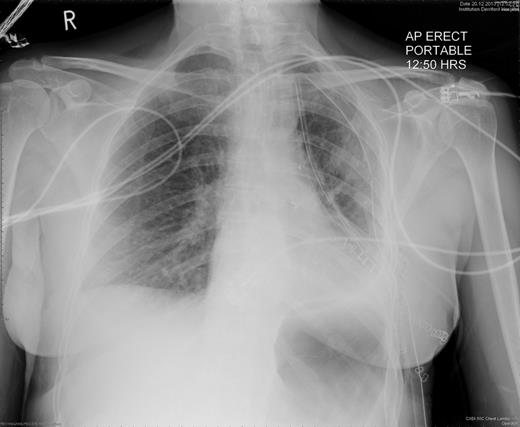
Chest radiography immediately after left upper lobectomy demonstrates good lower lobe expansion.
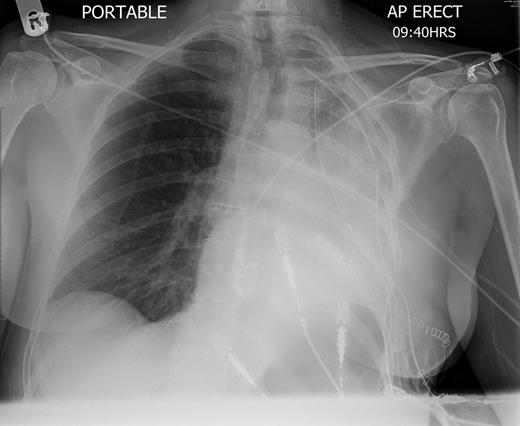
Chest radiography on the first post-operative day shows left-sided consolidation with normal left hemidiaphragm position.

CT scan shows acute angulation of left lung hilum with complete obstruction of left lower lobe bronchus.
DISCUSSION
Lung torsion is a very rare complication which may occur following trauma, any thoracic procedures and lobectomies [1–4]. It can lead to pulmonary infarction and lobar gangrene if left untreated. Right middle lobe is the most common lobe to undergo torsion after ipsilateral upper or lower lobectomy [3]. Torsion may lead to bronchial obstruction and pulmonary flow compromise which are associated with increased post-operative morbidity and mortality if left untreated. Causes of pulmonary torsion are not well defined. However, extensive dissection around the hilum, dissection of pulmonary ligament and complete interlobar fissure in the absence of pleural adhesions are the likely culprits for increased lobar mobility which predisposes to torsion.
A high index of suspicion is vital to diagnose lung torsion following lung resection. Sudden unexplained dyspnoea or tachypnoea refractory to oxygenation even with normal arterial blood gases and haemoptysis are the most common alarming symptoms. Chest radiograph showing sudden consolidation and reduced expansion of the previously normal lobe along with mediastinal shift to the contralateral side raises the suspicion of lobar torsion. Persistent consolidation after urgent physiotherapy manoeuvres may necessitate performing bronchoscopy to exclude endobronchial narrowing or obstruction. Emergency exploratory thoracotomy is necessary to confirm the diagnosis as the delay in detorsion might increase the likelihood of infective and thromboembolic complications and mortality. Treatment of lung torsion includes either detorsion and fixation or completion pneumonectomy. Pneumonectomy should not be performed at the exploratory thoracotomy if the affected lobe is thought to be viable especially if pulmonary function tests are not optimal for completion pneumonectomy. However, resection of the affected lobe should not be delayed if lobar infarction or gangrene is suspected. Good analgesia, aggressive antibiotics treatment and mini-tracheostomy to aid suctioning of secretions may help to reduce the infectious complications after torsion.
Lung torsion after lobectomy has been previously reported in all lobes. Exact mechanisms are unknown. Increased lobar mobility due to disruption of intrathoracic attachments is the likely cause. A high index of suspicion is essential for early recognition and definitive treatment.



