-
PDF
- Split View
-
Views
-
Cite
Cite
Junko Tokuno, Hiroyuki Cho, Keiji Yamanashi, Yuichiro Ueda, Ryota Sumitomo, Tsuyoshi Shoji, Cheng-Long Huang, A case of a resected thymoma in the middle mediastinum, Journal of Surgical Case Reports, Volume 2014, Issue 8, August 2014, rju077, https://doi.org/10.1093/jscr/rju077
Close - Share Icon Share
Abstract
We experienced an extremely rare case of a thymoma in the middle mediastinum. A 42-year-old woman presented with a 4-cm-sized abnormal mass in the middle mediastinum by chest computed tomography. To resect this tumor, we performed surgery using the thoracoscopic lateral approach from the right side subsequently followed by a median sternotomy. After the resection of this tumor, the intraoperative quick pathological examination diagnosed this tumor as a thymoma. An extended thymectomy was performed additionally.
INTRODUCTION
Thymoma in the middle mediastinum is extremely rare. A 42-year-old woman presented with an abnormal mass in the middle mediastinum by chest computed tomography (CT). To resect this tumor, we performed an operation using the thoracoscopic approach from the right side subsequently followed by a median sternotomy. Intraoperative quick pathological examination diagnosed this tumor as a thymoma. An extended thymectomy was performed additionally. We here discuss the treatment strategy for such cases.
CASE REPORT
A 42-year-old woman was referred to our department with an abnormal shadow found by chest CT during the treatment for pneumonia. After she had recovered from pneumonia with antibiotics, she was admitted for further examinations and surgery. She was asymptomatic and did not have any episodes of ptosis, diplopia, muscle weakness or exertional dyspnea.
A systemic examination revealed only a slight elevation of the serum acetylcholine receptor antibody level (1.6 nmol/l). However, other titers including several tumor markers were within the normal range.
Contrast-enhanced CT revealed a heterogeneous tumor measuring 4 cm in the middle mediastinum. The tumor was surrounded by many mediastinal structures, including brachiocephalic trunk, right brachiocephalic vein, superior vena cava (SVC), azygos vein, ascending aorta and trachea. However, its invasion to these mediastinal structures was uncertain (Fig. 1A and B). By magnetic resonance imaging (MRI), the tumor showed low intensity on both T1- and T2-weighted images, which means that this tumor was not cystic but solid (Fig. 1C and D). Positron emission tomography demonstrated that this tumor had no significant increased accumulation of FDG (SUV max 2.2–2.7). Considering these findings, this tumor was preoperatively suspected of being a neurogenic tumor or lymphoma due to its location.
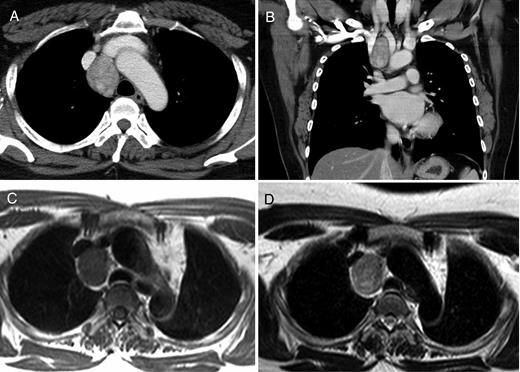
Contrast-enhanced CT revealed a heterogeneous tumor measuring 4 cm in the middle mediastinum (A and B). MRI showed a tumor demonstrating the low intensity both on the T1-weighted image (C) and the T2-weighted image (D).
To resect this tumor, we started surgery using the thoracoscopic lateral approach from the right side. There was no intrapleural adhesion or pleural effusion, and the tumor was easily detected in the mediastinum, behind the superior vena cava (SVC) anterior to the trachea. After opening of the superior mediastinal pleura, the azygos vein was dissected using Endo-GIA Tri-Staple camel 45 mm (Covidien, Dublin). Without any significant invasion to the adjacent mediastinal structures, it was possible to dissect the tumor from the trachea, SVC and right brachiocephalic vein (Fig. 2). However, the edge of this tumor was so deep that dissection of this tumor from the brachiocephalic trunk was impossible only with the right thoracoscopic lateral approach. Then, a subsequent median sternotomy was performed to remove this tumor. Intraoperative quick pathological examination diagnosed it as a thymoma. An extended thymectomy was performed additionally.
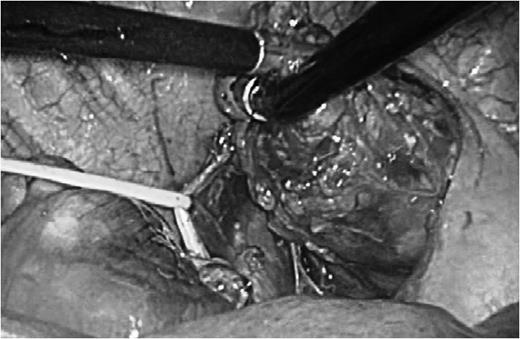
Intraoperative findings. Dissecting the tumor from surrounding structures. The vagus nerve was taped.
The tumor was yellowish and 4.9 cm at its largest diameter. A microscopic examination showed the tumor to contain spindle-shaped cells with a lymphocyte-rich component (Fig. 3). The postoperative pathological diagnosis was type AB of a thymoma according to the World Health Organization classification. The postoperative course was uneventful. The patient was discharged on postoperative Day 10. She was doing well at 12 months after surgery without recurrence of the tumor or any symptoms associated with myasthesia gravis.
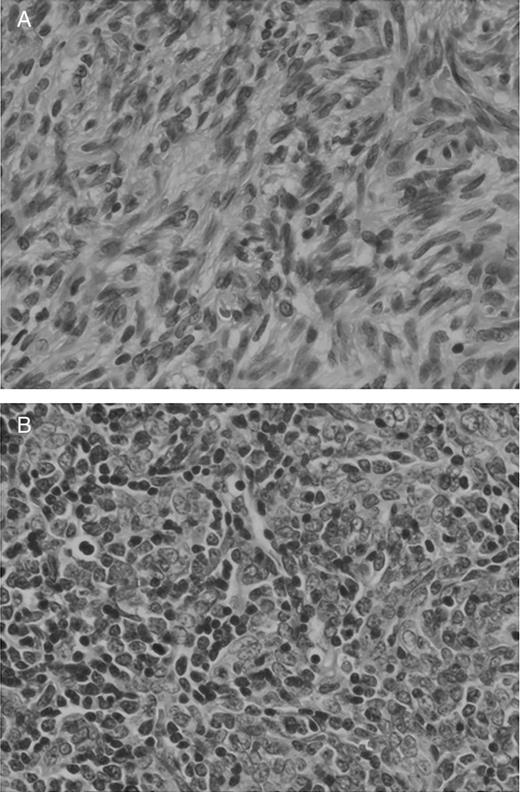
Pathological findings. Spindle cell proliferation (A) and lymphocyte infiltration (B) (hematoxylin eosin stain ×400).
DISCUSSION
Most thymomas are found in the anterior mediastinum because of the proper location of the thymus. In contrast, the most common site of thymoma is in the anterior mediastinum, and the sites of ectopic thymoma are the neck, the posterior mediastinum and pulmonary hilus [1, 2]. In particular, a thymoma occurring in the middle mediastinum is extremely rare and is considered to be associated with mismigration of thymic gland tissue during embryogenesis [4].
There have been several reports regarding the middle mediastinal thymoma [1–5]. Since it is difficult to establish the pathological diagnosis for tumors in the middle mediastinum preoperatively, in the present case, we chose surgery as the first line of the treatment because this tumor was solid with the possibility of malignancy.
In contrast, there have been only two reports about middle mediastinal thymoma with myasthesia gravis written in English [4, 5]. However, the preoperative acetylcholine receptor antibody level was also elevated in the present case. Since the elevation of the acetylcholine receptor antibody level is closely related to myasthesia gravis, the present case should be preoperatively considered as possible myasthesia gravis, especially in order to avoid the postoperative acute myasthesia gravis crisis.
Regarding the approach for surgery, two steps were used in this case. Preoperatively, we considered that this tumor could not be resected only by median sternotomy. Surgery was started by the lateral thoracoscopic approach. However, the edge of this tumor was so deep that the dissection of this tumor from the brachiocephalic trunk was impossible only with right thoracoscopic lateral approach. Therefore, a median sternotomy was performed subsequently. The two-step approach was considered to be necessary and safe for the resection of this tumor present in the middle mediastinum which is surrounded by many major structures.



