-
PDF
- Split View
-
Views
-
Cite
Cite
Anestis Hatzigeorgiadis, Konstantinos A. Boulas, Nikolaos Barettas, Konstantinos Blouhos, Bilateral primary spontaneous pneumothorax in an otherwise-healthy overweight young man, Journal of Surgical Case Reports, Volume 2014, Issue 8, August 2014, rju076, https://doi.org/10.1093/jscr/rju076
Close - Share Icon Share
Abstract
Bilateral primary spontaneous pneumothorax (BPSP) is a rare condition, accounting for ∼1.6% of spontaneous pneumothoraces. Patients with primary spontaneous pneumothorax have typically low body weight. BPSP in overweight/obese patients is an exceptionally rare event. The present report describes a case of an otherwise-healthy 20-year-old male patient with BMI 29.8 kg/m2 presented to our hospital owing to low-intensity chest pain and shortness of breath 7 days after the onset of symptoms. Plain chest X-ray revealed the presence of bilateral pneumothorax. Chest tubes were inserted on both sides. During hospitalization, a computed tomography demonstrated multiple blebs on the surface of the upper lobes of both lungs. Hereupon, the patient referred to a tertiary center and underwent elective single-stage minimally invasive bilateral video-assisted thoracoscopic surgery. The present case report shows that BPSP in overweight/obese patients is an existing condition.
INTRODUCTION
Pneumothorax is usually categorized into spontaneous and traumatic. Spontaneous pneumothorax (SP) comprises the largest group and is classified into primary spontaneous (PSP) and secondary spontaneous pneumothorax. PSP usually occurs in young, tall, thin men, especially smokers, in the absence of an underlying lung disease [1]. Although, SP is a relatively common condition, bilateral primary spontaneous pneumothorax (BPSP) is a very rare clinical condition with an occurrence ranging from 1.3 to 1.9% of all cases of SP [2]. Herein, we present a case of BPSP in an overweight young male patient, which is an exceptionally rare event.
CASE REPORT
An otherwise-healthy, non-smoker, 20-year-old, overweight (BMI 29.8 kg/m2) Greek male patient was presented to the emergency department complaining of low-intensity chest pain and breathlessness of progressive worsening over the preceding 7 days. On admission, physical examination revealed diminished breath sounds on both sides. Blood pressure was 125/70 mmHg, heart rate 100 beats/min, SaO2 97% on air and axillary temperature 36.8°C. Laboratory tests were normal. Initial plain chest X-ray demonstrated bilateral pneumothoraces (more prominent on the left side) and no deviation of the trachea (Fig. 1).
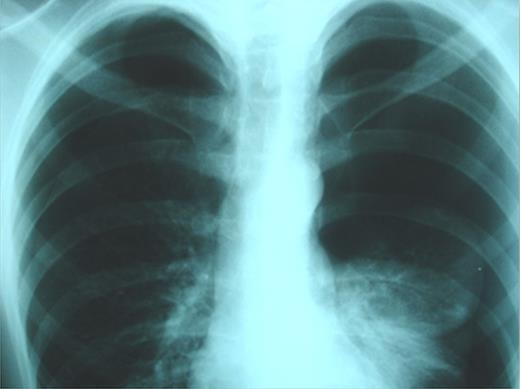
Plain chest X-rays on admission revealing bilateral pneumothorax.
On emergency basis, the patient was managed with bilateral tube thoracostomy through the fifth intercostal spaces. During hospitalization, both lungs were gradually expanded; the use of continuous aspiration was necessary for a couple of days, in order to achieve complete expansion of the left lung (Fig. 2). Both chest tubes were removed on the fifth day of hospitalization. Next day the plain X-ray revealed recurrence of pneumothorax on the left side (Fig. 3). A chest tube was reinserted. Continuous suction was used and complete expansion of the left lung was succeeded. The tube was removed after 5 days; no recurrence took place at this time. During the next 3 days the patient remained under observation; serial physical examinations and chest X-rays were normal and the patient was discharged home.

Complete bilateral lung expansion after insertion of chest tubes.

Recurrence of pneumothorax on the left side after removing the chest tube.
During hospitalization a chest computed tomography (CT) was performed and revealed the presence of blebs at the apices of both upper lungs (Fig. 4). After recovery the patient was referred to a tertiary center for an elective video-assisted thoracoscopic surgery intervention (VATS). Three years after, no recurrence of pneumothorax took place and the patient remains healthy.
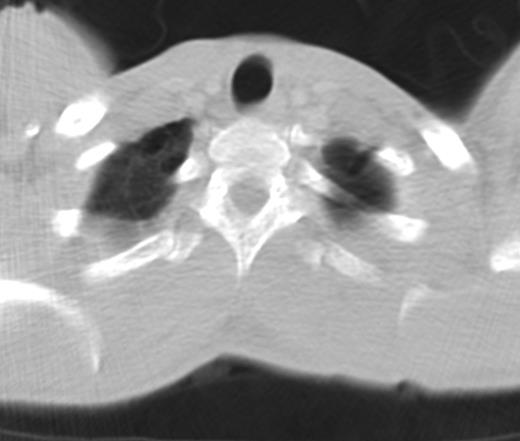
CT image showing bilateral blebs on the apices of the upper lobes.
DISCUSSION
SP is a relatively common condition in clinical practice. PSP usually occurs in the absence of any obvious underlying lung disease; however, blebs and bullae apparently play a role in the pathogenesis of PSP, as they are found on CT or during thoracoscopy or thoracotomy in 48–79% of these patients [3]. Diagnosis of bilateral pneumothorax presents difficulties; while unilateral pneumothorax is relatively easily suspected from the patient's medical history, physical and radiological findings, the diagnosis of bilateral pneumothorax is usually delayed. The presence of equally diminished breath sounds in both sides and the presence of a not deviated trachea often mislead clinicians and delay chest drain insertion which is usually performed after the transaction of chest CT [4].
Although SP is a relatively common condition, BPSP is a very rare clinical condition. Lee et al., in their study of the 616 patients with 807 episodes of PSP, found that the incidence of BPSP was 1.6% (13 patients). In univariate regression analysis, patients with PSP compared with patients with BPSP had significantly lower body weight, BMI, higher body height/body weight ratio and higher incidence of bilateral blebs/bullae seen in HRCT of the lung. However, in multiple regression analysis, only BMI and the presence of bilateral blebs/bullae retained statistically significant importance [5]. Huang et al. found that only lower BMI and smoking were significantly associated with the formation of BPSP. In their study, the proportion of bilateral blebs/bullae seen in HRCT was higher in the BPSP group than that in the PSP group (63 vs 53%, respectively), but the difference was not statistically significant (P = 0.724) [6]. The present report describes a case of BPSP in an overweight patient showing that PSP is an existing condition in patients with BMI value higher than the normal.
Chest drainage constitutes the basis of initial treatment [7]. Generally, if an SP affects <20% of one lung, observation is efficient; the absorption rate of the air is ∼1.25% (50–75 ml/day). If pneumothorax affects >20% of the lung or if it increases during observation, chest tube drainage may be required. Air leakage can be diminished in 5 h and in 48 h in 52 and 82% of patients with tube thoracostomies, respectively [8]. In patients with BPSP, one side should always be drained regardless of the extent of pneumothorax, whereas the other side can be managed by simple observation depending on the extent of the air in the pleura space. Prolonged air leakage is the most common indication for operation in the first episode of pneumothorax [9].
Today, VATS is accepted as a standard approach for the surgical treatment of SP. Compared with open thoracotomy, this procedure provides visualization of the entire thoracic cavity by video and causes less postoperative pain. Single-stage bilateral VATS procedure for BPSP has been advocated as an elective procedure to avoid subsequent anesthetic and operative procedures and longer hospital stays. If any underlying pulmonary disease is detected during surgical treatment, the existence of pleural communications should be investigated and mediastinal pleura should be examined carefully. Bullectomy is the most effective method for preventing recurrences. In addition, apical pleurodesis further reduces the risk of recurrence [10]. In our case, the patient was successfully managed initially with a bilateral tube thoracostomy and finally with an elective bilateral VATS procedure.
In conclusion, BPSP is a rare clinical condition and usually develops in patients with low BMI and bilateral blebs/bullae. BPSP in overweight-obese patients is an existing condition and its early diagnosis requires high suspicion index. BPSP needs urgent assessment and management, followed by bilateral single-stage VATS treatment as a safe and effective procedure.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.



