-
PDF
- Split View
-
Views
-
Cite
Cite
Rajendraprasad R. Butala, Manit Arora, Ashith A. Rao, Prakash D. Samant, Sunirmal Mukherjee, A rare case of ipsilateral shoulder and thumb CMC joint neuropathic arthropathy, Journal of Surgical Case Reports, Volume 2014, Issue 6, June 2014, rju054, https://doi.org/10.1093/jscr/rju054
Close - Share Icon Share
Abstract
Neuropathic arthropathy (Charcot joints) most frequently affect the weight-bearing joints of the body, are commonly associated with a variety of medical and neurological conditions and are notoriously difficult to treat due to the nature of the underlying pathology. We present a case of ipsilateral shoulder and thumb carpometacarpal (CMC) joint neuropathic arthropathy secondary to cervical syringomyelia. To our knowledge, this is the first reported case in the literature of this rare association.
INTRODUCTION
Neuropathic arthropathies, also known as Charcot joints, have been commonly reported in medical and neurological conditions such as diabetic neuropathy, tertiary syphilis, cerebral palsy, syringomyelia and spinal cord injury, among others. The common factor is a sensory deficit in the affected extremity [1]. The Charcot joint lacks the ability to respond via reflexes to abnormal stress. Consequently, the subchondral bone of the involved joint disintegrates, leading to joint collapse and considerable joint deformity. The usual clinical manifestation of a neuroarthropathy is a pain-free joint or mild discomfort, if any, and the symptoms are disproportionately mild in relation to the degree of destructive joint changes seen radiographically [2].
The joints most frequently affected are the weight-bearing joints, predominantly the mid-foot but also the ankle, knee, hip and elbow. In his review of 118 cases of neuropathic arthropathy, Johnson [3] suggested that the pattern of involvement was dependent on the underlying neurological condition—in tabes dorsalis, the knee was predominantly affected; in syringomyelia, the upper extremity joints; and in diabetes, the foot and ankle joints. To our knowledge, there have been no reported cases of neuropathic arthropathy of the CMC joint of the thumb and the ipsilateral shoulder. We present a case of neuropathic arthropathy of the upper extremity, including the CMC joint of the thumb and the ipsilateral shoulder, secondary to syringomyelia.
CASE REPORT
A 53-year-old, right-hand-dominant housewife presented to our institution with insidious onset of painless stiffness of the upper extremity joints for a period of 3 years on a background of paraesthesia and weakness in the left upper limb for a period of 6 years. There was an increase in joint stiffness, weakness and paraesthesia over the last 3 years.
The patient complained of weakness and intermittent paraesthesia to the left upper extremity for a period of 6 years which had been worsening over the last 3 years. The paraesthesia was vague in nature and non-dermatomal in distribution. The patient subsequently complained of a dull ache in the left shoulder over the last 3 years with overhead activities and sleeping on the affected shoulder at night, relieved by rest and paracetamol. This ache was followed by stiffness in the left shoulder restricting her daily activities since the last 2 years. The patient also complained of stiffness to the left thumb over the same period, with a reduction in the ability to grasp and grip objects. There was no history of contralateral limb symptoms, difficulty walking, problems with balance or gait, bowel or bladder problems, or morning stiffness. There was no history of constitutional symptoms such as fever, lethargy, night sweats, weight loss or anorexia. There was no history of trauma or heavy weight lifting over the last 6 years. There was no history of previous tuberculosis, degenerative or rheumatoid arthropathy, poliomyelitis, neurological conditions or diabetes.
On examination of the left shoulder, the patient had severe restriction of active shoulder movement with flexion of 80°, extension of 20°, external rotation of 50° and internal rotation of 20°. Active abduction was limited to 90° and was painless (Fig. 1). Passive range of movements was essentially normal and painless. There was no localized tenderness, local warmth or swelling. Neurological testing revealed normal tone, sluggish reflexes, power of grade 4 in the left upper limb with decreased sensation to pain, fine touch and temperature, suggestive of C3–C8 involvement. Proprioception and deep touch, however, was intact.

Clinical photograph of passive (left) and active (right) abduction of the left shoulder joint.
Examination of left hand revealed volar subluxation of the first CMC joint of the thumb, with a reduced range of motion in all directions. However, there was no tenderness, local warmth or swelling to the same. There was wasting of the intrinsic muscles of the left hand. Higher centre, cerebellar, neck, elbow and lower limb neurological examination were essentially normal.
Laboratory investigation revealed an elevated serum alkaline phosphatase (257.7) and an elevated CRP (26.2). There was no anaemia, leucocytosis, elevated blood sugars, elevated liver or kidney function tests or elevated ESR.
We further evaluated the patient using radiographs of the shoulder (Fig. 2) and thumb (Fig. 3) which confirmed our suspicion of neuropathic arthropathy. To exclude Milwaukee shoulder as a cause of the severe changes observed on the shoulder radiograph, we performed an MRI of the shoulder which revealed an intact rotator cuff (Fig. 4). Further, due to the associated neurological symptoms in the left upper limb, we performed an MRI of the cervical spine (Fig. 5) to identify any underlying neurological pathology. This MRI revealed a multi-level cervical syringomyelia.
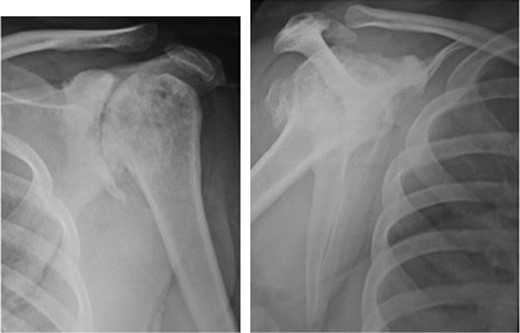
Antero-posterior and scapular radiograph of the left shoulder joint showing severe reduction in glenohumeral joint space, slight superior subluxation of the humeral head, severe subchondral sclerosis and osteophytic changes, subchondral cysts and change in shape of the humeral head. Loose bodies were also present.

Posterio-anterior and oblique photograph of the left thumb showing severe arthritic changes in the first CMC joint with severe reduction in joint space, volar subluxation, subchondral sclerosis, osteophytic changes and loose bodies.
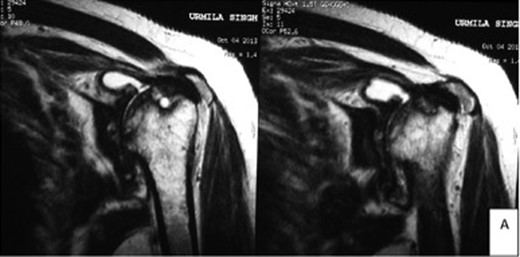
MRI of the left shoulder joint confirming severe arthritic changes, including synovial thickening and destruction of the shape of the humeral head. The rotator cuff was essentially normal with only slight degenerative changes.
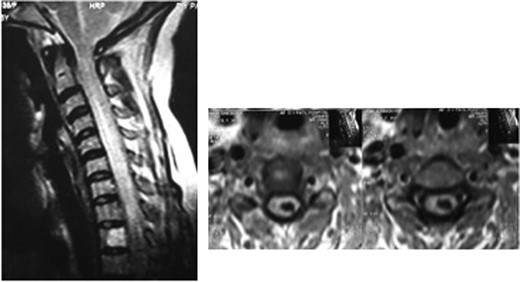
Cervical spine MRI showing a multi-level syringomyelia of the cervical spine.
Overall, our findings were suggestive of neuropathic arthropathy of the left shoulder and left CMC joint secondary to cervical syringomyelia.
Owing to the non-dominant hand involvement, stage of disease and unequivocal results of surgery in the literature (see Discussion), we undertook non-operative management of the patient consisting of medications (anti-inflammatory, analgesia and antacid), orthoses (thumb spica splint application at night), patient education (avoidance of aggravating factors and repetitive stress) and physiotherapy (shoulder and thumb range of motion and gentle stretching exercises). At 6 months post-therapy, the patient had a 60% reduction in symptoms, and had no further progression of arthropathy on range of motion testing.
DISCUSSION
Neuropathic arthropathy of the CMC joint is a rare condition with no cases reported in the literature. Neuropathic arthropathy of the shoulder, although more common (occurring in 5% of cases), is still rare. Involvement of the hand joints is extremely rare with only a handful of cases reported in the literature [4]. Neuroarthropathies are more common in the weight-bearing joints, such as the knee, hip, foot and ankle [2]. Up to 25% of cases of neuropathic arthropathy are caused by syringomyelia, although there is no reported case of ipsilateral shoulder and CMC joint involvement. There is report of ipsilateral shoulder and elbow neuroarthropathy secondary to syringomyelia [5]. Neuropathic arthropathy of the elbow joint is most common after syringomyelia.
The syrinx interrupts the decussating fibres of the lateral spinothalamic tract that mediates pain and thermal sense while sparing fibres that mediate sensate of deep touch and proprioception, causing a dissociated segmental anaesthesia. Loss of deep tendon reflexes and weakness with or without atrophy of the upper limb musculature may also be present [5].
The exact pathogenesis of neuroarthropathies is controversial. The ‘neurotraumatic’ theory postulates that the normal pain mechanism is deactivated by articular denervation, allowing repetitive trauma to occur. If the joint remains unprotected, rapid destruction, hemarthrosis, synovial thickening and secondary ligament laxity ensue [6]. The ‘neurovascular’ theory postulates that underlying neurological changes lead to hypervascularity in the subchondral bone [2]. There may be extensive erosion of the bone, increased bone resorption, bone weakening, microfractures and subchondral collapse and destruction of the joint [7].
Neuropathic arthropathy progresses in three stages [7] (Fig. 6).
![Stages of neuroarthropathy. (Adapted from Giurini et al. [8].)](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2014/6/10.1093_jscr_rju054/2/m_rju05406.jpeg?Expires=1772271979&Signature=X5SXSOueOZzVJfkQcBvkiAcqicMDo2uZtI5tpuBM-Yn4muuqvlVrq1T1xu9nwvjJfIntPCG5YLvOBn5DvfM6gr78~r~gW1K90rRzHebPzmaGSVFgTcyIgz62E4Ndr1Rz1QSllzUdGxlPft0i9XSTBGFvF6Y5IpXSxhaHKamUVDOK~VKJAo1JooBXmU2dNd7Dcaa7e4vnu2KfPETrMTgUUpRdjPU5HLCj1ynNWSOGO2czJd4kyf0JQPQuAf~xCadgC95UOZCjMFoobfTmkPm2MhzW99e-lT7NE3stcIUponTC5iuvf~KFjafmKp5KWozfI6zDHzBga53NWp7FO7HgIw__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
Stages of neuroarthropathy. (Adapted from Giurini et al. [8].)
Accordingly, our patient had Stage I neuroarthropathy of the left CMC and left shoulder joints. Radiographically, neuroarthropathies are classified as either atrophic or proliferative [2]. The atrophic form is characterized by substantial bone resorption and near disintegration of the joint [7]. This form is classically asymptomatic. The proliferative, and more common, form is characterized by significant joint destruction, periarticular new bone formation, bony fragments and fractures, osteophyte formation and ultimately fusion [8]. Both the involved joints in our patient are radiographically suggestive of the proliferative type.
Treatment goals are to reduce further articular damage while retaining a functional joint. Initially conservative measures are adopted, including symptomatic treatment, anti-inflammatory medications, orthotics, weight-bearing reduction techniques and patient education to minimize mechanical trauma [9]. Recently, several studies have demonstrated a beneficial effect of bisphosponates in the treatment of neuropathic joints [10]. Failure of conservative measures is an indication for surgical intervention. Surgical options include prosthetic replacements, resection arthroplasty and arthrodesis. Previously reported treatment option for the neuroarthropathic shoulder includes humeral head prosthetic replacement [9]. However, arthroplasty in a neuropathic joint is theoretically a poor option due to lack of protective pain sensation and reflexes, presence of osteopenic bone and the weakness of surrounding ligaments and musculature. This leads to high stress of implanted components and subsequent loosening and periprosthetic fractures. Historically, arthrodesis of neuropathic joints also has poor results; however, the use of internal fixation devices may improve outcomes when compared with external fixation [8]. As there are no reported cases of CMC neuroarthropathy, no specific indications exist in this literature. Our management methodology leads to cessation of clinical progression of the disease.



