-
PDF
- Split View
-
Views
-
Cite
Cite
Waddah Arafat, Costantine Albany, Thomas M. Ulbright, Richard Foster, Lawrence H. Einhorn, Very late relapse of germ cell tumor as a teratoma: a case report and review of the literature, Journal of Surgical Case Reports, Volume 2014, Issue 6, June 2014, rju051, https://doi.org/10.1093/jscr/rju051
Close - Share Icon Share
Abstract
Very late relapses of germ cell tumors (GCTs) are rare. There are few reports of relapses occurring beyond 20 years of initial treatment. Here we describe a case of a very late relapse of Stage I testicular non-seminomatous germ cell tumor 27 years after orchiectomy. The relapse presented as a retroperitoneal mass in the precaval lymph nodes with negative tumor markers. It was resected and pathology confirmed it as metastatic teratoma. This case emphasizes the importance of lifelong surveillance for patients with GCTs.
INTRODUCTION
Germ cell tumors represent the most common cancer in men aged 15–35 years [1]. The prognosis of metastatic testicular germ cell tumor has dramatically improved after the introduction of cisplatin-based chemotherapy in the 1970s. More than 95% of patients with metastatic GCT are cured with cisplatin-based chemotherapy with or without the need for surgical resection of residual disease. However, ∼10% of patients who achieve disease-free status recur, with the vast majority developing within 2 years of initial treatment. However, 2–3% present with late relapses, which by definition occur at least 2 years after successful treatment, with the retroperitoneum being the most frequent site. These tumors are rarely curable by chemotherapy. Surgical resection is the preferred treatment for late relapse [2].
CASE REPORT
A 42-year-old patient with a history of clinical Stage I testicular non-seminomatous germ cell tumor (NSGCT) status post-left radical orchiectomy in 1986 (the exact pathology from his orchiectomy was not available) without additional treatment presented with right testis, back and flank pain. An abdominal computed tomography (CT) scan showed a retroperitoneal mass measuring 11.3 × 9.3 × 4.6 cm in the precaval area (Fig. 1) with negative tumor markers including β-HCG and alpha-fetoprotein. The patient underwent a testicular ultrasound of the right testis that showed microlithiasis but no hypodense mass. An exploratory laparoscopy with biopsy showed morphological features suggesting retroperitoneal idiopathic fibrosis. However, the clinical and imaging features as assessed by the urologist and oncologist were felt to be inconsistent with this possibility. The patient, therefore, underwent a CT-guided fine needle aspiration of the mass that showed extensively necrotic tumor.

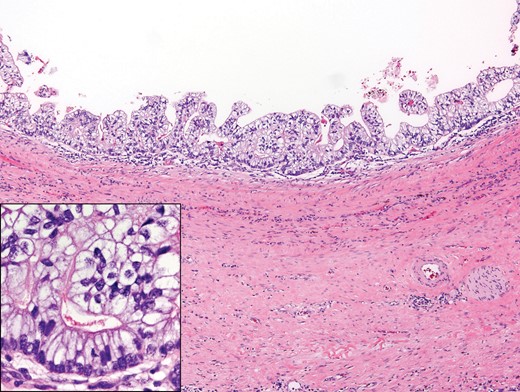
An open laparotomy with resection of the mass and the retroperitoneal lymph nodes in a non-nerve sparing manner was performed. The pathological examination showed metastatic teratoma, with the lesion consisting of several cysts lined by stratified, mildly atypical glandular epithelial cells forming small papillae and encircled by smooth muscle (Fig. 2). Dense, fibrosclerotic and inflamed stroma was present peripheral to the mass. Immunohistochemical stains were positive for SALL4, supporting germ cell tumor origin and also positive for EMA, arguing against the possibility of yolk sac tumor.
DISCUSSION
This is a very rare and challenging case presentation. First, very late relapse of NSGCT with pure teratoma 27 years after orchiectomy is unusual. Secondly, inadequate sampling of the retroperitoneal lesion led to a misinterpretation suggesting retroperitoneal fibrosis. This disease, however, does not produce a discrete mass but a diffuse thickening of retroperitoneal soft tissue and was considered incompatible with the imaging findings, as determined by review of our urologist. Only after resection was the lesion confirmed as teratoma. It is difficult to tell whether this case represent a late relapse of a clinical Stage I NSGCT or a new extragonadal GCT. The exact location of the retroperitoneal mass, whether interaortocaval or periaortic, was difficult to judge because of its large size. There was, therefore, ambiguity concerning the possibilities of an extra-gonadal primary (midline) or metastasis (left periaortic).
Very late relapses of GCT are rare and only a few cases of relapses happening >20 years after the initial presentation are reported in the literature [3–11].
This case emphasizes the importance of life-time surveillance of patients with GCT. Even patients with extremely low risk for late relapse, including those with clinical Stage I disease, still need lifelong follow-up. Most late relapses are in patients with advanced disease, who have been treated with chemotherapy and have post-chemotherapy retroperitoneal lymph node dissection-containing teratoma.



