-
PDF
- Split View
-
Views
-
Cite
Cite
Elroy P. Weledji, Adolphe Elong, Vincent Verla, Secondary repair of severe chronic fourth-degree perineal tear due to obstetric trauma, Journal of Surgical Case Reports, Volume 2014, Issue 5, May 2014, rju034, https://doi.org/10.1093/jscr/rju034
Close - Share Icon Share
Abstract
Obstetric injury is the commonest cause of anal incontinence. We report a case of anal incontinence as a result of severe chronic fourth-degree perineal tear secondary to birthing with complete disruption of the perineum. Secondary repair consisting of an anterior sphincter repair and levatorplasty in a poor resourced area rendered excellent immediate clinical result. The outcome of anterior sphincter repair following obstetric trauma is good but long-term follow-up is required because of the underlying complexity of obstetric injury. As prevention is not always possible, immediate recognition and adequate primary treatment is of importance.
INTRODUCTION
Obstetric injury is the most common cause of sphincter injury and pelvic floor failure resulting in lack of bowel control. The pudendal nerve may be damaged during the course of prolonged vaginal delivery consequent to stretching [1–3]. 4 to 6% of women who have vaginal deliveries will suffer from faecal incontinence [1]. A third/fourth-degree tear (involving the anal sphincter complex) occurs in 0.5–2%. Eighty five per cent will have a persistent defect of the sphincter despite the immediate (primary) repair by the obstetrician [2]. Conservative treatment (diet/medical manipulation, biofeedback and pelvic floor exercises) can be successful. Secondary repair is usually offered to patients with gross faecal incontinence [4, 5]. The outcome depends on the extent of the anal sphincter damage and associated neurological injury [5].
CASE REPORT
A 32-year-old woman was admitted electively for the management of a 2-year history of anal incontinence following a traumatic vaginal delivery of her second child. She had undergone a manual forceful dilatation of the posterior vagina for cephalo-pelvic disproportion which resulted to a severe perineal tear. This was repaired but she complained of severe urgency of defaecation and flatus incontinence since then. She had awareness of the need to defaecate but was unable to retain solid stool for more than a few minutes. Reduced anal sensation for liquid stool and faecal perianal soiling followed a high residue diet. She had severe discomfort and soiling during sexual intercourse because of the very close proximity of the anal canal to the vagina. Her faecal incontinence score was 15/20 according to the Cleveland Clinic scoring system [i.e. Solids (usually) 3, Liquids (always) 4, Flatus (always) 4, use of pad (never) 0, lifestyle alteration (always) 4]. Physical examination revealed a patulous anus immediately adjacent to the posterior for chette of the vagina indicating a poor internal sphincter function (Fig. 1). She had a lax external sphincter tone on voluntary squeezing and the anorectal angle was weakly accentuated with squeeze. Proctoscopy revealed an empty rectum and normal mucosa. A preoperative diagnosis of a fourth-degree perineal tear involving the internal anal sphincter (IAS) and external anal sphincter (EAS) with possible mild pudendal neuropathy was made and she consented to a perineal repair (Table 1).
| First degree | Injury to perineal skin |
| Second degree | Injury to perineum involving perineal muscles but not involving the anal sphincters |
| Third degree | Injury to perineum involving the anal sphincter complex: 3a: <50% of ext anal sphincter thickness 3b: >50% EAS thickness 3c: both EAS and IAS involved |
| Fourth degree | Involves anal sphincter complex (EAS and IAS) and anorectal mucosa. |
| First degree | Injury to perineal skin |
| Second degree | Injury to perineum involving perineal muscles but not involving the anal sphincters |
| Third degree | Injury to perineum involving the anal sphincter complex: 3a: <50% of ext anal sphincter thickness 3b: >50% EAS thickness 3c: both EAS and IAS involved |
| Fourth degree | Involves anal sphincter complex (EAS and IAS) and anorectal mucosa. |
| First degree | Injury to perineal skin |
| Second degree | Injury to perineum involving perineal muscles but not involving the anal sphincters |
| Third degree | Injury to perineum involving the anal sphincter complex: 3a: <50% of ext anal sphincter thickness 3b: >50% EAS thickness 3c: both EAS and IAS involved |
| Fourth degree | Involves anal sphincter complex (EAS and IAS) and anorectal mucosa. |
| First degree | Injury to perineal skin |
| Second degree | Injury to perineum involving perineal muscles but not involving the anal sphincters |
| Third degree | Injury to perineum involving the anal sphincter complex: 3a: <50% of ext anal sphincter thickness 3b: >50% EAS thickness 3c: both EAS and IAS involved |
| Fourth degree | Involves anal sphincter complex (EAS and IAS) and anorectal mucosa. |

A severe chronic fourth-degree tear secondary to birthing with grossly deficient perineum (—a thin demarcation between anus and vagina). Preoperative examination.
Following mechanical bowel preparation and i/v prophylactic antibiotics (ceftriaxone 1 gm and metronidazole 500 mg) given prior to induction of anaesthesia, and, with the patient in the lithotomy position a proctoscopy was carried out to irrigate the rectum. The dissection was commenced laterally out in the ischiorectal fat to establish an appropriate plane and proceeded towards the site of sphincter injury which was in the anterior margin. The anodermal flap was carefully mobilized from the vagina by sharp dissection in a cephalad direction to expose the entire length of the injury with the plane lying posterior to any large paravaginal veins (Fig. 2). The edges of the damaged sphincter muscle were identified and the plane between the anal mucosa and the muscle on either side was developed. As the injury extended proximally into the levator ani (puborectalis) muscle, an anterior levatorplasty was performed by plicating the anterior limbs of the muscle to the midline with 2-0 polyglactin sutures (Fig. 3). This opposed the pelvic floor in the midline anteriorly and reconstructed the perineal body. The anterior defect of the IAS extended through the anal mucosa and was plicated with 2-0 polygalactin suture (Fig. 3). The vaginal wall was plicated with interrupted sutures of 3-0 polygalactin to provide added support to the rectovaginal septum. An overlapping repair of ∼3 cm of the mobilized edges of the external sphincter extended the length of the anal canal and was performed using five horizontal mattress sutures of 2-0 polygalactin (Fig. 4). Following irrigation and haemostasis the semi-circular skin wound which has now almost become longitudinal was closed in an inverted ‘Y’ fashion. The distance between the posterior forchette and the anal canal was seen to be lengthened (Fig. 5). Postoperatively, sitz baths were instituted and the patient was given a low-residue diet for the first 48 h. Apart from constipation relieved with microlax enema, she made good recovery with no signs of wound infection nor haematoma. Postoperatively, her anal tone at rest was increased and there was reasonable increase in the maximum squeeze pressure. Her incontinence score a week after repair was 2/20, i.e. solids (never) 0, liquids (never) 0, flatus (sometimes) 2, use of pad (never) 0, lifestyle alteration (never) 0. She was discharged on the 10th postoperative day and long-term follow-up planned (Table 2).
| . | Never . | Rarely . | Sometimes . | Usually . | Always . |
|---|---|---|---|---|---|
| Solids | 0 | 1 | 2 | 3 | 4 |
| Liquids | 0 | 1 | 2 | 3 | 4 |
| Flatus | 0 | 1 | 2 | 3 | 4 |
| Use of pad | 0 | 1 | 2 | 3 | 4 |
| Lifestyle alteration | 0 | 1 | 2 | 3 | 4 |
| . | Never . | Rarely . | Sometimes . | Usually . | Always . |
|---|---|---|---|---|---|
| Solids | 0 | 1 | 2 | 3 | 4 |
| Liquids | 0 | 1 | 2 | 3 | 4 |
| Flatus | 0 | 1 | 2 | 3 | 4 |
| Use of pad | 0 | 1 | 2 | 3 | 4 |
| Lifestyle alteration | 0 | 1 | 2 | 3 | 4 |
Rarely: less than once a month; sometimes: more than once per month or less than once a week; usually: more than once a week but less than once a day; always: more than once a day.
CCIS 0, perfect continence; CCIS 1–7, good continence; CCIS 8–14, moderate incontinence; CCIS 15–20, severe incontinence; CCIS >20, completely incontinent.
| . | Never . | Rarely . | Sometimes . | Usually . | Always . |
|---|---|---|---|---|---|
| Solids | 0 | 1 | 2 | 3 | 4 |
| Liquids | 0 | 1 | 2 | 3 | 4 |
| Flatus | 0 | 1 | 2 | 3 | 4 |
| Use of pad | 0 | 1 | 2 | 3 | 4 |
| Lifestyle alteration | 0 | 1 | 2 | 3 | 4 |
| . | Never . | Rarely . | Sometimes . | Usually . | Always . |
|---|---|---|---|---|---|
| Solids | 0 | 1 | 2 | 3 | 4 |
| Liquids | 0 | 1 | 2 | 3 | 4 |
| Flatus | 0 | 1 | 2 | 3 | 4 |
| Use of pad | 0 | 1 | 2 | 3 | 4 |
| Lifestyle alteration | 0 | 1 | 2 | 3 | 4 |
Rarely: less than once a month; sometimes: more than once per month or less than once a week; usually: more than once a week but less than once a day; always: more than once a day.
CCIS 0, perfect continence; CCIS 1–7, good continence; CCIS 8–14, moderate incontinence; CCIS 15–20, severe incontinence; CCIS >20, completely incontinent.
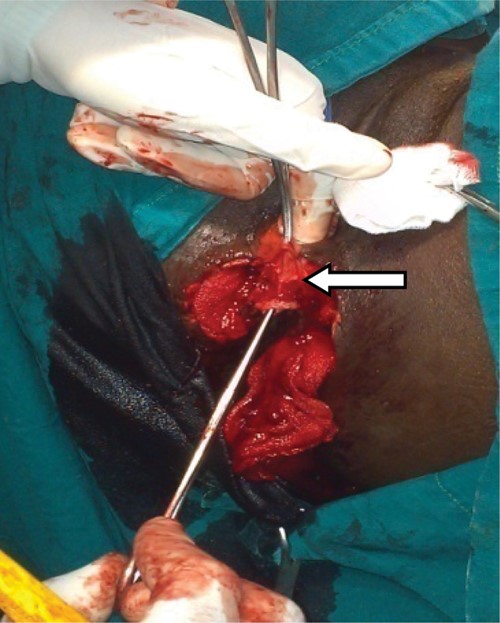
Vagina carefully separated from the anterior rectal wall (arrow); gauze swab in the right and left ischioanal fossa, respectively.
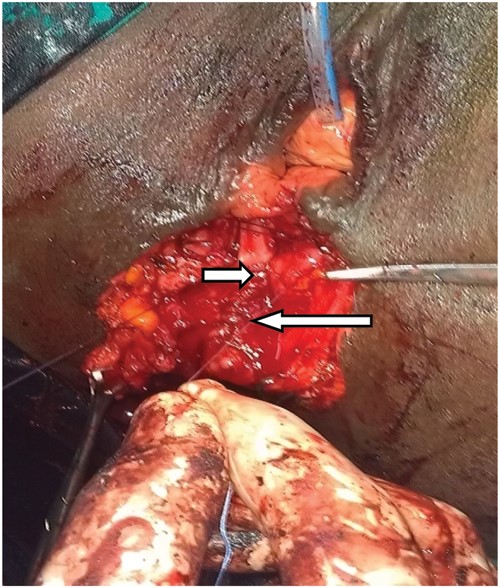
IAS plication (long arrow) extending to the plicated levator ani (short arrow) (forceps on the separated external sphincter, urethral catheter in situ).
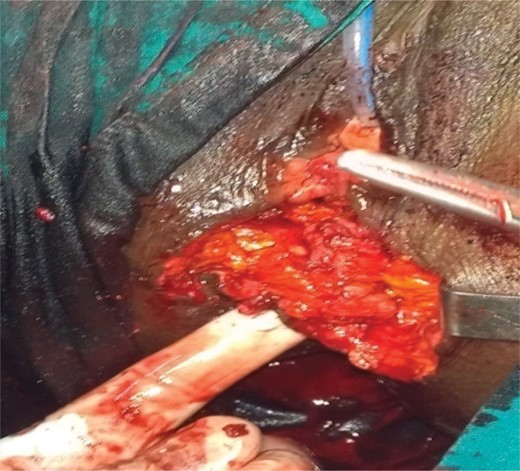
Anterior external sphincteroplasty (covered by isciorectal fat; finger in anal canal).

Wound closed in an inverted ‘Y′-shaped manner with elongation of the skin over the perineal body (arrow-anal canal; deeply-seated anal verge with increase length of anal canal).
DISCUSSION
Primary repair is ideal as successful primary sphincteroplasty substantially improves quality of life and reduces overall cost of treatment [6]. Following primary repair a poor continence score at 3 months post-partum, usually with urge incontinence of faeces denotes severe anal sphincter dysfunction and is a predictive factor for persistent faecal incontinence [7]. In a resourced area, endoanal ultrasound will localize the injury site and size the extent of sphincter damage prior to a secondary repair [4, 5]. Anorectal physiology is useful for patients not considered for operative repair so as to obtain baseline information and, to determine the extent of anal sphincter damage and identify pudendal neuropathy in candidates for surgery [4, 5, 7, 8]. Operative management is usually offered to a patient with a score of 12 or greater, an underlying correctable abnormality and gross faecal continence [4, 5, 8]. These range from an overlapping EAS repair for a distal sphincter defect to repair of the entire pelvic floor for neuropathic faecal incontinence [4, 5]. Where IAS injury can be identified, it is advisable to repair separately [9]. The prognosis following EAS repair is good with 60–80% asymptomatic at 12 months [5]. Improvement in the functional length of the sphincter corresponded to a successful outcome [4, 5, 7, 8]. Unfortunately, more recent studies have demonstrated that only ∼40% remain satisfactorily continent [5]. Patients with coexisting pudendal neuropathy or operative pudendal nerve damage will be at risk and may benefit from sacral nerve stimulation or a neosphincter procedure or even an end-stoma [4, 5, 7]. Long-term follow-up is thus required [2, 6]. It should be compared with long-term results following a structured training in recognizing and repairing sphincter injury primarily.
Consent
‘Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the editor of this journal’.
AUTHORS’ CONTRIBUTIONS
E.P.W. is the main author and surgeon. A.E. gave obstetric advice in the discussion, V.V. is the anaesthetist and gave advice on pain control.
CONFLICT OF INTEREST
The authors declare that they have no competing interests.
ACKNOWLEDGEMENTS
We thank the patient for giving us her consent to publish this case report. We thank the senior medical students Sr Quinta Mua and Samain Nkendo for providing the images, and the theatre and surgical nursing staff of the Regional hospital Buea for their perioperative care of the patient. We hope the success of this case will encourage the formation of an anal incontinence clinic in the hospital.



