-
PDF
- Split View
-
Views
-
Cite
Cite
Ahmad Mahamid, Meir Mizrahi, Chamutal Gur, Tomer Adar, Exacerbation of left ventricular outlet obstruction in hypertrophic obstructive cardiomyopathy: an unexpected complication of gastric banding, Journal of Surgical Case Reports, Volume 2014, Issue 5, May 2014, rju040, https://doi.org/10.1093/jscr/rju040
Close - Share Icon Share
Abstract
Hypertrophic obstructive cardiomyopathy (HOCM) is characterized by a dynamic left ventricular outlet tract (LVOT) obstruction, which may be exacerbated by reduced preload and Valsalva. Laparoscopic adjustable gastric band (LAGB) placement is a restrictive bariatric procedure which may be complicated by recurrent vomiting and Valsalva. Pre-operative cardiac evaluation of patients scheduled for LAGB usually focuses on ischemic heart disease. Reported here is the case of a 64-year-old female admitted for evaluation of recurrent pre-syncopal episodes. The patient was diagnosed with HOCM with a significant increase in an LVOT pressure gradient during Valsalva. Thus, recurrent vomiting secondary to LAGB exacerbated a pre-existing cardiomyopathy. Symptoms resolved after gastric band deflation. This is the first report of such a complication after LAGB, demonstrating the hemodynamics of HOCM in a unique setting and underscoring the need for a structural cardiac assessment prior to bariatric surgery.
INTRODUCTION
Hypertrophic obstructive cardiomyopathy (HOCM) is characterized by left ventricular hypertrophy including asymmetric septal hypertrophy (ASH) and a systolic anterior motion of the anterior mitral valve leaflet which results in left ventricular outlet obstruction. The clinical manifestations of HOCM are variable, ranging from asymptomatic, to chest pain, dyspnea on exertion and syncope. In accordance with the Venturi effect, left ventricular outlet tract (LVOT) obstruction in HOCM is dynamic, and may be exacerbated by decreased preload or afterload and increased inotropy of the left ventricle. In some patients, the measured LVOT pressure gradients are within the normal range or only slightly elevated at rest, with considerable increase after exercise or during the Valsalva maneuver [1, 2].
Bariatric surgery is the most effective way to maintain a significant weight reduction in the long term [3, 4]. The laparoscopic adjustable gastric banding (LAGB) procedure has gained worldwide popularity. LAGB is a bariatric procedure during which a band is placed around the stomach, restricting food intake [5, 6].
Postoperative complications for LAGB include migration of the band, band slippage and dilatation of the pouch, esophageal dilatation, dysmotility and gastro-esophageal reflux disease (GERD). LAGB-induced esophageal dilation occurs in 14% of cases, and may contribute to more frequent symptoms of reflux and emesis [7, 8]. Vomiting is one of the most common side effects of LAGB.
We report an unusual case of a female patient who developed an exacerbation of LVOT pressure gradient in HOCM after intense vomiting, caused by tightening of her gastric band.
CASE REPORT
A 64-year-old female was admitted to our medical center due to recurrent episodes of pre-syncope. The patient denied any connection to postural changes, dyspnea, palpitations or urinary complaints, and she associated the episodes with prolonged standing and strenuous work at home.
The patient had undergone LAGB for morbid obesity 5 years prior to admission, with a weight reduction of ∼65 kg. The patient suffered from recurrent vomiting and GERD attributed to her tightened gastric band. The patient's past medical history was positive for ischemic heart disease, empty sella syndrome, primary hyperaldosteronism, polymyalgia rheumatica, fatty liver, osteoporosis, peptic ulcer disease and status post-deep vein thrombosis.
On physical examination an ejection type systolic murmur was heard, with radiation to the neck and a subtle bruit of both the carotid arteries.
Blood tests demonstrated: mild hypokalemia 3.2 (3.5–5 mmol/l), elevated creatinine 130 (60–106 micromol/l) and urea 9 (3.3–6.5 mmol/l), and normocytic anemia with hemoglobin 10.8 (12–16 g % female).
Electrocardiogram was remarkable for Q waves in leads I, aVL and V6. Chest X-ray (CXR) demonstrated a marked esophageal distention with an air fluid level (Figs 1 and 2).
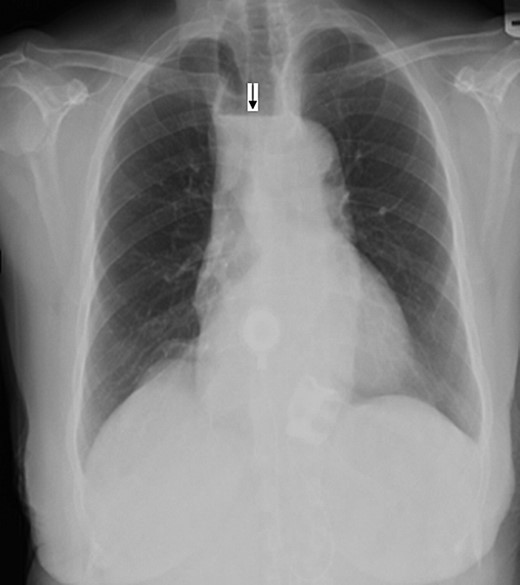
Anterio-posterior CXR views demonstrate the shadow of a dilated esophagus and air fluid level (black arrow).
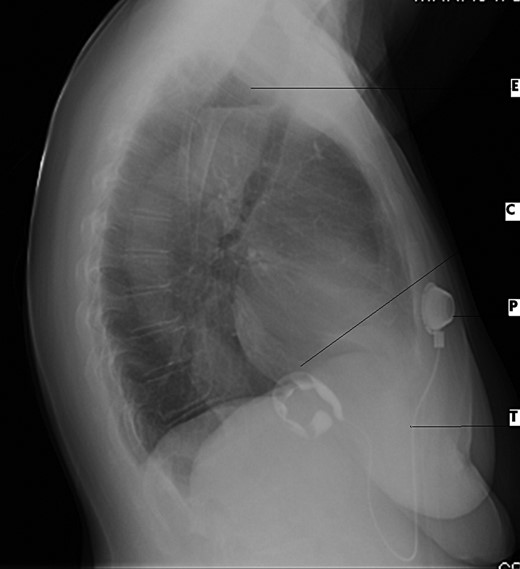
Lateral CXR view demonstrates dilated esophagus and fluid air level (E), contrast medium-filled inflatable inner cuff (C), connecting silicone tube (T) and subcutaneous sutured radiopaque access port (P).
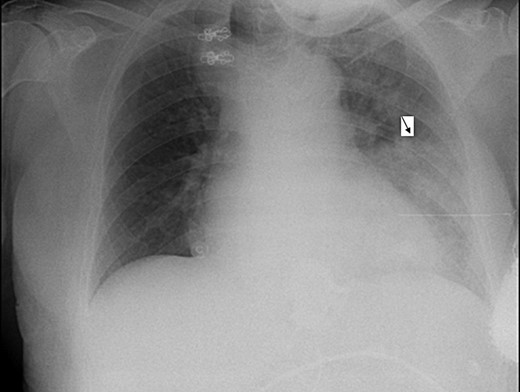
During her hospitalization, the patient developed fever and desaturation, with a new infiltrate on CXR (Fig. 3). She was diagnosed with pneumonia and was treated with antibiotics. Later on, after significant improvement, though still suffering from a barking cough (attributed to reflux), the patient left her bed and in an attack of severe coughing, lost consciousness, fell and became cyanotic. Repeated attempts to improve oxygenation failed until a naso-gastric tube was inserted with drainage of ∼1 l of non-bilious content, resulting in rapid improvement in the patient's condition. A repeat CXR revealed the naso-gastric tube in her esophagus. Repeated attempts to insert the NGT into her stomach failed, even with the aid of contrast media. The silastic band was then deflated, allowing for less restriction, and an endoscopy showed esophagitis but no obstruction.
On syncope workup, Doppler assessment of the carotid artery revealed no significant obstructions, and echocardiogram demonstrated a small left ventricular cavity with hyper contractile global systolic function, mild basal septal hypertrophy and LVOT obstruction with the pressure gradient increasing from 16 mmHg at rest to 120 mmHg during Valsalva (Fig. 4).
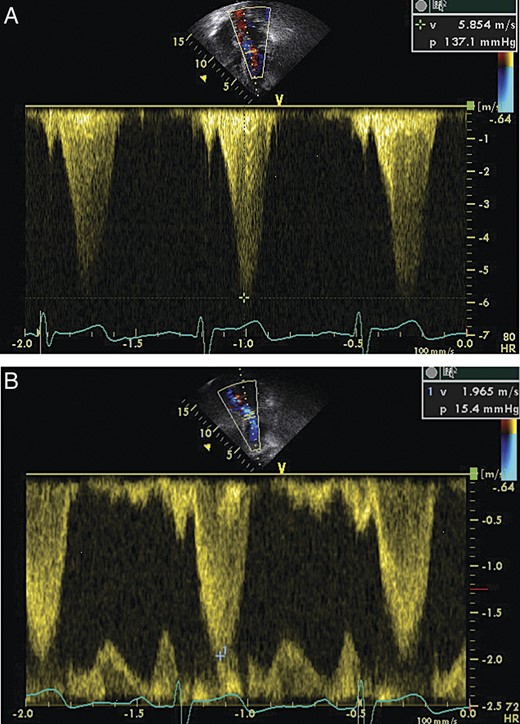
(A) Echocardiogram demonstrating LVOT flow parameters at rest. (B) Echocardiogram demonstrating LVOT flow parameters during Valsalva maneuver, note the increase in amplitude and the ‘dagger-shaped’ flow pattern demonstrating the dynamics of LVOT obstruction.
In light of the echocardiographic findings, the patient's recurrent pre-syncope was attributed to LVOT obstruction exacerbated by Valsalva and hypovolemia (in a patient with recurrent vomiting) secondary to gastric banding. Adding to this chronic condition, acute infection and retching resulted in an acute and almost fatal exacerbation. This condition responded to esophageal decompression with resolution of the retching and relief from recurrent Valsalva. Treatment with β-blockers was initiated, diuretics were discontinued and the patient was referred to the cardiomyopathy clinic. On follow-up, several months later, the patient reported the resolution of pre-syncopal feelings though she had gained several pounds in weight.
DISCUSSION
LAGB is a widely used modality for the treatment of morbid obesity. Several complications have been reported, including band occlusion. The etiology includes a too tight band, and patients experience symptoms of reflux (heartburn), nausea and vomiting. A contrast meal verifies the diagnosis. Therapy consists of immediate band deflation and NGT placement.
This case highlights a rare and unreported complication of the LAGB procedure, which mainly presented as pre-syncope and dizziness, in a patient with HOCM.
The patient suffered from a unique combination of two separate clinical conditions, in which an unknown cardiomyopathy was exacerbated by recurrent vomiting which in itself was associated with hypovolemia and Valsalva. A grave deterioration in the patient's condition was observed when a concurrent respiratory infection induced a positive inotropic effect. All these resulted in decreased left ventricular filling and increased LVOT obstruction. Symptoms were relieved after the gastric band was loosened, proving the pathogenetic link between dynamic LVOT obstruction and gastric banding.
This emphasizes the importance of pre-operative cardiac evaluation of candidates for gastric banding, which should not be limited to evaluation of ischemic heart disease and must also include a structural assessment. Demonstration of ASH should be considered at the very least a relative contraindication for gastric banding, with LVOT pressure gradient dynamics during Valsalva being a crucial determinant factor.
CONFLICT OF INTEREST
None.



