-
PDF
- Split View
-
Views
-
Cite
Cite
Rachael Lauren Armstrong, Phillip Bradford Heyse, Gastropleural fistula in metastatic ovarian cancer, Journal of Surgical Case Reports, Volume 2014, Issue 5, May 2014, rju033, https://doi.org/10.1093/jscr/rju033
Close - Share Icon Share
Abstract
Gastropleural fistula is a rare condition, most frequently reported as a result of trauma, peptic ulcer disease or malignancy. We report a case of gastropleural fistula in a patient with metastatic ovarian cancer who presented with hydropneumothorax and mediastinal shift. She was successfully managed with an open partial gastrectomy, repair of diaphragmatic defect, and thoracoscopic washout and decortication. Based on our case and review of the literature, surgical repair of gastropleural fistula should be considered as a palliative procedure even in patients with end-stage cancer.
INTRODUCTION
Gastropleural fistula is a rare condition, most frequently reported as a result of trauma, peptic ulcer disease or malignancy. We report a case of gastropleural fistula in a patient with metastatic ovarian cancer who presented with hydropneumothorax and mediastinal shift.
CASE REPORT
A 69-year-old female with Stage IV ovarian cancer status post-total abdominal hysterectomy, bilateral salpingo-oophorectomy, appendectomy, tumor debulking and eight cycles of carboplatin and paclitaxel presented with sudden onset of dyspnea. She reported a 4-month history of mild dyspnea and pleurisy, which had been attributed to previously diagnosed, cytology-proven bilateral malignant pleural effusions. She was also being treated for bilateral lower extremity Deep venous thromboses with warfarin. Computed tomography (CT) chest demonstrated a left hydropneumothorax with mediastinal shift (Fig. 1). Thoracostomy tube was placed with tea-colored drainage on insertion. She was intubated the following day for respiratory failure.
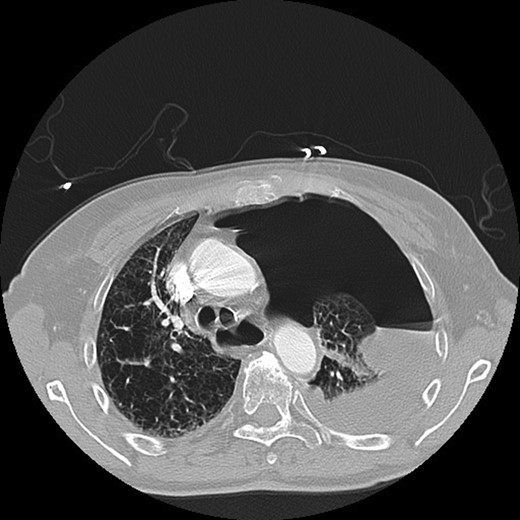
CT chest demonstrating left hydropneumothorax with mediastinal shift.
Bilious drainage was noted from her chest tube. An upper GI series with gastrografin demonstrated a gastropleural fistula (Fig. 2). General surgery was consulted for possible surgical management. The patient was started on total parental nutrition, broad-spectrum antibiotics and antifungal therapy. Her respiratory status improved and she was extubated on hospital Day 4.
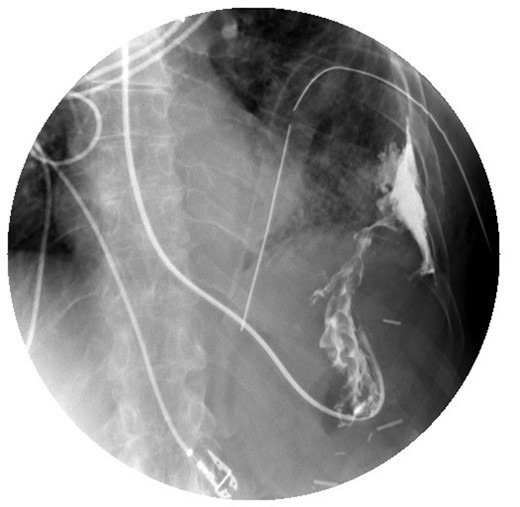
Upper GI study demonstrating contrast administered via nasogastric tube with extravasation into the pleural space.
A discussion with the patient and multidisciplinary treatment team, including surgical oncology, gynecologic oncology and cardiothoracic surgery took place regarding possible surgical intervention. The patient was agreeable to palliative surgery to address the gastropleural fistula and its attendant complications.
After 2 weeks of broad-spectrum antibiotics, antifungal therapy, bowel rest and Total parenteral nutrition, she was taken to the operating room. A gastropleural fistula was identified involving the gastric fundus to the left diaphragm. The fistula was taken down and the gastric defect was closed with a linear stapler. The diaphragm was repaired with a bovine pericardial patch via our abdominal approach. On further exploration of the abdomen, a serosal abnormality was noted on the surface of the gallbladder; cholecystectomy was performed and demonstrated one lymph node within the gallbladder specimen containing metastatic poorly differentiated carcinoma. A Stamm gastrostomy was performed and the abdomen closed. Decortication, washout and chest tube drainage of the left chest was then performed by video-assisted thoracoscopic surgery.
The patient was extubated postoperatively. Oral intake was initiated on postoperative Day 3. Her chest tubes were discontinued on postoperative Days 5 and 8. Due to poor appetite and oral intake, supplemental gastrostomy tube feedings were initiated. She was discharged on postoperative Day 13, and went on to receive additional chemotherapy. She eventually opted for Hospice care and passed away 6 months later.
DISCUSSION
Gastropleural fistulas are an uncommon condition, most often reported in the literature as a complication of traumatic diaphragmatic rupture, gastric perforation due to peptic ulcer disease or malignancy. Other etiologies include previous surgery, such as lobectomy [1] or splenectomy [2] or an infection abutting the diaphragm, such as a subdiaphragmatic abscess or empyema [3]. Gastropleural fistulas require surgical management, as conservative management generally fails and can progress to sepsis and death.
Due to its rare nature, diagnosis of gastropleural fistula requires a high index of suspicion. Most common presentations include upper abdominal pain, left chest pain, hydropneumothorax, or most significantly, tension pneumothorax [4]. Initial workup includes chest roentgenogram, which may demonstrate pneumothorax or pleural effusion. Upper GI series shows enteral contrast from the stomach entering the pleural cavity. CT scan may demonstrate enteral contrast in the pleural space. After thoracostomy tube placement, the presence of gastric secretions, food particulate or bile should raise the suspicion for gastropleural fistula.
Successful surgical management of gastropleural fistula has been reported with both laparoscopic and open methods, and frequently requires a combined thoracic and abdominal approach for partial gastric resection, diaphragmatic repair, and washout and drainage of the chest. Endoscopic repair with vicryl mesh and fibrin glue has also been reported [5]. In our patient, extensive washout and decortication of the chest was indicated, requiring thoracoscopy in addition to open resection of the fistula and diaphragmatic repair.
There have been few reported cases of gastropleural fistula in the setting of malignancy without direct extension or involvement of the tumor, two in renal cell carcinoma and one in recurrent ovarian cancer. In one patient, the gastropleural fistula was thought to be the result of concomitant radiation and chemotherapy [6]. In two reported cases, the patient had been treated with bevacizumab, which has been associated with an increased incidence of fistula formation [7, 8].
Perforation of gastric tumor into the pleural space has been reported in cases of lymphoma [9] and Ewing's sarcoma [10] as the inciting event leading to gastropleural fistula. At the time of her index operation, our patient had intraluminal metastatic disease of the jejunum, as well as extraluminal metastatic disease of the transverse colon. It is likely that the gastric perforation resulting in gastropleural fistula was attributable to ovarian cancer metastasis, although the gastric specimen did not demonstrate evidence of tumor involvement.
In our patient, surgical repair was successful, allowing her recovery from sepsis, improved respiratory status, and eventual discharge. In this case, operative intervention resulted in short-term survival from her acute disease and a marked improvement in her quality of life.
In conclusion, surgical repair of gastropleural fistula in the setting of metastatic cancer should be considered. Resolution of the sequela of the fistula leads to increased quality of life as well as the opportunity to continue adjuvant therapy and perhaps allow for an increased long-term survival.



