-
PDF
- Split View
-
Views
-
Cite
Cite
Lyle Burdine, Keith Lai, Jonathan A. Laryea, Ipilimumab-induced colonic perforation, Journal of Surgical Case Reports, Volume 2014, Issue 3, March 2014, rju010, https://doi.org/10.1093/jscr/rju010
Close - Share Icon Share
Abstract
Biologic immune modulators such as ipilimumab have demonstrated the efficacy against metastatic melanoma. We present a recent case of a 52-year-old male who initially developed mild colitis following the initiation of ipilimumab treatment for metastatic melanoma. Despite initial improvement with immediate cessation of drug and initiation of high-dose steroid therapy his clinical condition worsened and the patient presented to our facility in extremis from colonic perforation. Following an extended right hemicolectomy his postoperative period was extended due to continued symptomatic enteritis. After 3 weeks colonoscopy revealed that the autoimmune event had begun to subside; his condition improved, resulting in discharge. We discuss this particular side effect with respect to ipilimumab adjuvant therapy in melanoma.
INTRODUCTION
Immunotherapy has emerged over the last decade as an effective adjuvant therapy for metastatic melanoma, a disease that has been relatively resistant to traditional therapeutic approaches. The goal of this therapy is to subvert cancer-mediated immune tolerance via the reduction of the activation threshold for T-cell mediated attack of tumor cells. With this goal in mind ipilimumab, a humanized IgG monoclonal antibody that blocks cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4), was approved for adjuvant therapy to improve survival in patients with metastatic melanoma [1–3]. The side effects of such an approach are of course predictable. Namely, lowering the immune tolerance for cancer cells will likely result in T-cell mediated attack of normal tissue, i.e. drug-induced autoimmunity. This article is a case report regarding one such event, ipilimumab-induced colitis.
CASE REPORT
A 52-year-old male with a history of Stage IIIb melanoma initially underwent a wide local excision with a sentinel lymph node biopsy for a 2.1 mm in-depth melanotic lesion of his left upper arm melanoma. The sentinel lymph node biopsy at that time was negative for malignancy. Two years later he returned with an in-transit metastasis proximal to the original lesion. He underwent re-excision and axillary lymph dissection at that time. Following the removal of this lesion he was started on ipilimumab at 6 mg/kg. He had completed two injections spaced 1 month apart before he returning to clinic with complaints of diarrhea and significant abdominal pain. At that time a CT scan (Fig. 1) and colonoscopy with biopsy were performed, both were consistent with active colitis. Adjuvant therapy was suspended and the patient was started on prednisone at standard dosage. The patient’s symptoms improved over the course of the next week. However, 2 weeks following initiation of immunosuppresion he presented acutely to the emergency department with hypotension, peritonitis and free air beneath the diaphragm. He was taken to the operating room for exploratory laparotomy. Following entrance to the abdomen via a midline incision extensive inflammation was noted from the terminal ileum to the mid-transverse colon. Perforation of the cecum was the salient finding (Fig. 2). A right extended hemicolectomy was performed with end ileosotomy. Pathology was consistent with ipilimumab-induced perforation colitis (Fig. 3). The patient tolerated the procedure and was cared for in the surgical intensive care unit overnight before being released to the general surgery floor in the morning. His postoperative course was complicated by continued symptomatic enteritis for the next 2 weeks; however by Week 3 repeat colonoscopy revealed evidence of regeneration and healing of the colonic mucosa. He was discharged home and will likely be scheduled for ileostomy takedown in 6–8 weeks following cessation of immunosuppression.
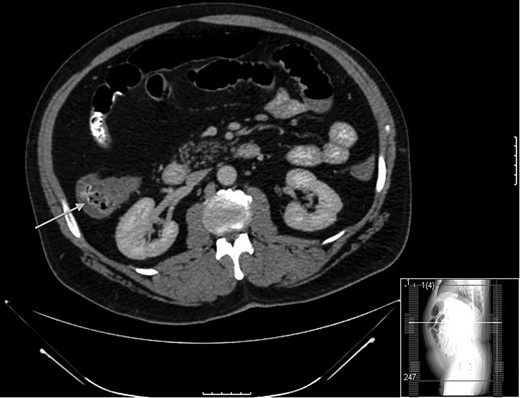
Thickening observed on CT scan at the time of initial presentation. Note the arrow pointing to cecum on axial section.
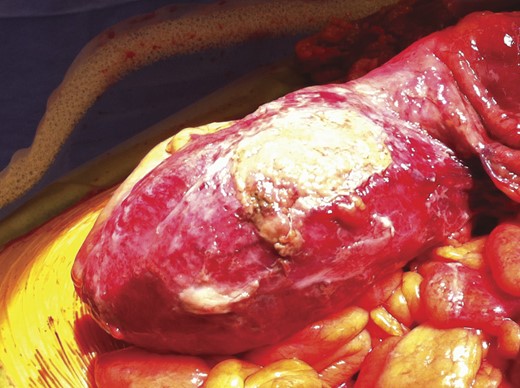
Cecal perforation identified at the time of operation. Gross inflammation observed from the ileocecal junction to the mid-transverse colon.
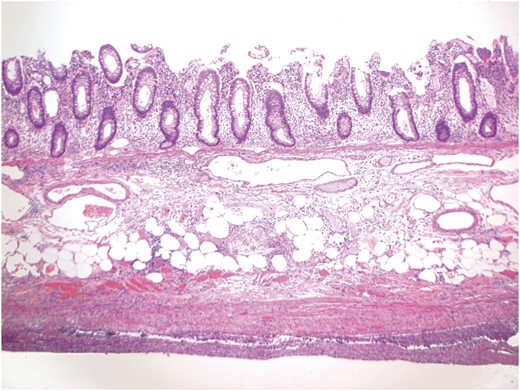
A representative section showing inflammation involving all layers of the colonic wall. The submucosal layer is slightly edematous, while the muscular layer is attenuated. The prominent acute and chronic inflammation involving the pericolonic soft tissue and peritonealized surface is consistent with the clinical impression of perforation.
DISCUSSION
Immunotherapy has proved to be one of the most effective therapies for metastatic melanoma [1]. Blocking attenuation of the T-cell arm of the adaptive immune system reduces the ability of cancer cells to evade the immune system has been the goal of this therapy since the outset [2]. Ipilimumab, a fully human, IgG1 monoclonal antibody blocks CTLA-4 and improves overall survival in patients with advanced melanoma [3, 4]. The predictable side effect can carry significant morbidity, as evidenced by this case. Given the fact that the half-life of the drug is 15 days, one can expect a prolonged postoperative course [5]. Initial clinical trials that proved the effectiveness of the drug demonstrated that colitis occurs in 30% of patients [6, 7], with roughly 10% of those patients with colitis requiring surgical intervention. The morbidity associated with this type of treatment is likely acceptable when balanced against certain mortality with metastatic melanoma. It is remarkable that the inflammation pattern seen in this case mirrors that observed in patients with severe Crohn's disease, namely intense inflammation at the ileocolic junction [8]. Moreover, severe cases of ipilimumab-induced colitis have been successfully treated with the biologic infliximab. Importantly, perforating drug-induced colitis will likely increase as the use of immunotherapy increases for melanoma and other chemo-resistant cancers becomes more prevalent.



