-
PDF
- Split View
-
Views
-
Cite
Cite
Tze Yeong Teng, Cheryl Chien-Li Lau, Unusual cause of pneumomediastinum in a laparoscopic extraperitoneal inguinal hernia repair, Journal of Surgical Case Reports, Volume 2014, Issue 10, October 2014, rju106, https://doi.org/10.1093/jscr/rju106
Close - Share Icon Share
Abstract
Pneumomediastinum is an extremely rare complication after laparoscopic inguinal hernia repair. Very few cases have been reported in the surgical literature to date and most reports indicate pneumoperitoneum from the transabdominal preperitoneal approach as a causative factor. This case report describes a patient in whom an elective total extraperitoneal inguinal hernia repair was complicated by a pneumomediastinum without concomitant pneumoperitoneum, and identifies the tracking of air along the anterior extraperitoneal space and endothoracic fascia as a cause. Previous case reports were reviewed and possible etiologies are discussed.
INTRODUCTION
Isolated pneumomediastinum after laparoscopic inguinal hernia repair is a rare complication and is most commonly due to tracking of air through congenital diaphragmatic defects from a pneumoperitoneum. A pneumoperitoneum is expected in a transabdominal preperitoneal approach or an inadvertent peritoneal breach in a total extraperitoneal (TEP) approach. We report a case of pneumomediastinum secondary to air tracking along the fascia transversalis and endothoracic fascia after laparoscopic hernia repair.
CASE REPORT
A 42-year-old male with a past medical history of hypertension was admitted for an elective TEP repair of his left inguinal hernia. Endotracheal intubation and general anesthesia were given uneventfully. The extraperitoneal space was developed with a balloon space maker, and insufflation of carbon dioxide at a maximum pressure of 12 mmHg was performed. Intraoperatively, a large incarcerated indirect left inguinal hernia containing omentum was reduced. A Optilene mesh (10 × 12 cm) was placed and tacked appropriately after hernia reduction. There were no obvious tears in the peritoneum and the total operative time was ∼90 min. No elevation of end-tidal CO2 was noted during the surgery and the patient was extubated successfully. The patient subsequently complained of left-sided chest pain on the same night of the surgery. He did not have abdominal pain. He had subcutaneous crepitus extending from the left groin to the left chest. His cardiac enzymes were negative and his electrocardiography revealed a sinus rhythm with no acute ischemic changes. A plain radiograph of the chest showed a sliver of lucency in the mediastinum suspicious for pneumomediastinum, with no obvious pneumoperitoneum or pneumothorax seen (Fig. 1). Computed tomographic (CT) imaging of the thorax and abdomen confirmed the radiograph finding of pneumomediastinum and diffuse subcutaneous emphysema tracking along the abdominal muscles bilaterally, as well as a small amount of free air and stranding in the left posterior pararenal space (Figs 2–4). The patient was treated conservatively with oral analgesia and supplemental oxygen. His chest pain resolved by the third postoperative day and he was discharged well. He was advised to avoid air travel for 1 month. He was reviewed in clinic at the 1-week and 1-month intervals and did not report any further chest pain or respiratory symptoms. His operation site healed well and he remained recurrence free.
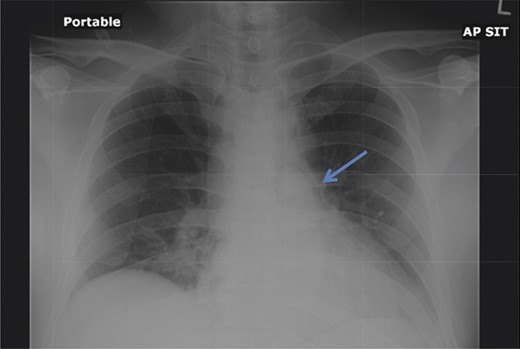
Chest radiograph demonstrates a pneumomediastinum (arrowhead).

Axial section CT pulmonary angiogram shows a pneumomediastinum (arrowhead).
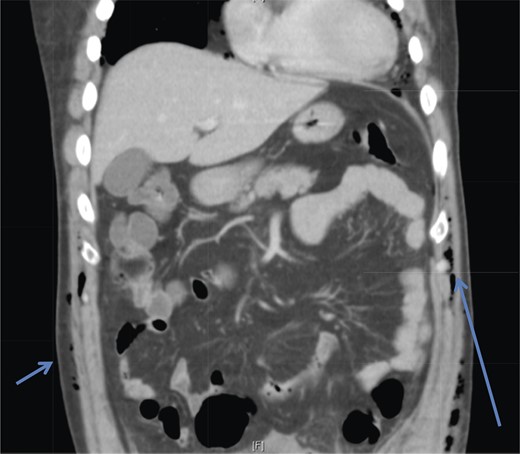
Coronal section CT abdomen scan demonstrates tracking of subcutaneous emphysema (arrowheads).
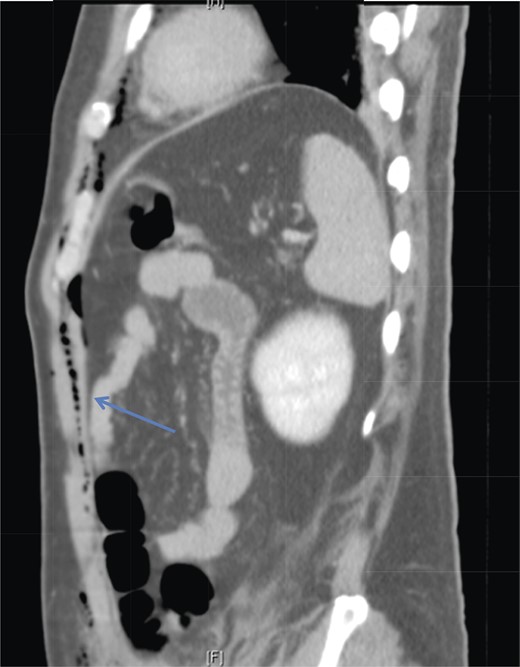
Sagittal section of CT abdomen demonstrates air tracking along the anterior extraperitoneal space (arrowhead) into the anterior mediastinum and preperitoneal fat.
DISCUSSION
Laparoscopic repair of inguinal hernias in an elective setting is becoming increasingly popular compared with open repair due to the advantages of decreased postoperative pain and faster return to employment activity. Known adverse outcomes of laparoscopic hernia repair include postoperative neuralgia, seroma and hematoma formation. However, pneumomediastinum is a rare complication, with fewer than 10 cases reported worldwide in the available literature. The actual incidence of pneumomediastinum after TEP inguinal hernia repair is unknown, as chest radiographs are not routinely performed after uncomplicated laparoscopic inguinal hernia repairs unless patients become symptomatic. Air may enter the mediastinum from the esophagus, trachea, bronchi, lungs, abdomen and also the retroperitoneal space, resulting in a pneumomediastinum.
Pneumomediastinum as a complication of TEP inguinal hernia repair usually occurs secondary to an inadvertent breach of the peritoneum, leading to a pneumoperitoneum and tracking of air into the mediastinum, and can occur even after repair of the peritoneal defect [1, 2]. Carbon dioxide (CO2) may enter the thoracic cavity from the abdominal cavity during intra-abdominal laparoscopic procedures through pleuroperitoneal hiatus (Bochdalek foramen), congenital diaphragmatic hernias (foramen of Morgagni) or damage to the falciform ligament [3, 4]. The incidence rate of pneumomediastinum is 18% after paraesophageal hernia repair and the presence of a pneumomediastinum after fundoplication is often recognized as a normal finding, illustrating that the esophageal hiatus is another possible route for tracking of air into the mediastinum [5]. High working CO2 insufflation pressures and prolonged length of surgery are also associated with the development of pneumomediastinum [6]. This is unlikely to be the case in our patient as surgery duration was not prolonged and the insufflation pressure was not high.
Laparoscopic CO2 can enter the retroperitoneal space and track along tissue planes into the pleural space and mediastinum [4]. Chien and Soifer [7] reported a case of pharyngeal emphysema complicating a laparoscopic hernia repair, and postulated that myopectineal dissection may lead to CO2 tracking retroperitoneally into the thorax. This is a possible cause of pneumomediastinum in our patient, as his CT imaging showed the presence of left posterior pararenal stranding, supporting a possible retroperitoneal dissection of CO2 to the thoracic cavity. Another pathway for transdiaphragmatic extension of air into the mediastinal space was proposed by Meyers [8]. The endothoracic fascia is continuous with the extraperitoneal space of the fascia transversalis. Extraperitoneal gas can dissect through the anterior gaps of the diaphragm between the sternal, xiphoid and costal origins of the diaphragm. With the aid of anatomical studies in cadavers, Kleinman et al. confirmed these observations [6]. This potential pathway likely explains the entry of CO2 from our patient's abdominal wall (extraperitoneal space) into the mediastinum, without the presence of pneumoperitoneum.
While pneumomediastinum has the potential to lead to cardiorespiratory compromise, our patient did not require any invasive ventilation and his symptoms resolved with medications and supplemental oxygen. This outcome is similar to Madan et al. [1] who reported that their patient did not require mechanical ventilation and recovered uneventfully. Browne et al., however, reported that their patient required a period of positive pressure ventilation before resolution of the pneumomediastinum [9]. Lo et al. reviewed several case reports of pneumomediastinum after laparoscopic inguinal repair and reported that only two of seven patients required an intercostal catheter insertion [10]. Fortunately, there have been no reports of mortalities secondary to pneumomediastinum as a complication of laparoscopic inguinal hernia repair.
In summary, pneumomediastinum complicating a laparoscopic inguinal hernia repair can lead to potential cardiorespiratory distress and surgeons should be cognizant of this rare occurrence. Radiological investigations are required to rule out pneumothorax and pneumoperitoneum. Most affected patients are hemodynamically stable and only require close monitoring as the pneumomediastinum will resolve without invasive therapy.
CONFLICT OF INTEREST STATEMENT
None declared.



