-
PDF
- Split View
-
Views
-
Cite
Cite
Marco Fabricio Bombón Caizaluisa, Héctor Daniel Montes, Luis Francisco Llerena Freire, Kevin Elías Albuja Delgado, Guido Panchana Coello, Transanal minimally invasive surgery for a rectal tubulovillous adenoma with high-grade dysplasia: a case report, Journal of Surgical Case Reports, Volume 2026, Issue 2, February 2026, rjaf931, https://doi.org/10.1093/jscr/rjaf931
Close - Share Icon Share
Abstract
We presented the case of a 48-year-old woman with a history of thyroid cancer under treatment, who was referred for evaluation of a long-standing sensation of a foreign body in the anal region, associated with occasional rectal bleeding. Physical examination and rigid rectoscopy revealed a polypoid lesion 3–4 cm from the anal verge. Laboratory tests were within normal limits. Pelvic magnetic resonance imaging (MRI) showed a solid, stenosing lesion 27 mm from the anal verge, infiltrating the muscular layer without mesorectal fascia involvement, measuring 73 mm longitudinally and 51 mm in both anteroposterior and transverse diameters, classified as a mid-to-low rectal tumor T3N0M0. Initial biopsy demonstrated a tubular adenoma with focal high-grade dysplasia and extensive low-grade dysplasia. Given the MRI findings suggesting invasion, colonoscopy with targeted biopsy was performed, confirming a tubular adenoma with high-grade dysplasia. The patient underwent transanal minimally invasive surgery (TAMIS), with complete excision of a friable, irregular lesion ~5 cm in diameter. Final histology reported a tubulovillous adenoma with focal high-grade dysplasia and low-grade dysplasia, with clear resection margins. Postoperative recovery was uneventful, and the patient remains asymptomatic during follow-up. This case highlights the role of TAMIS as a safe and effective organ-preserving technique for selected rectal adenomas with high-grade dysplasia, allowing complete excision and rapid recovery.
Introduction
Local excision remains a cornerstone in the management of benign rectal adenomas and selected early-stage rectal cancers. Conventional transanal excision (TAE) has been widely used; however, it presents technical limitations, particularly in accessing mid- and upper-rectal lesions due to restricted visualization and limited instrument maneuverability [1].
Introduced by Atallah et al. in 2010, transanal minimally invasive surgery (TAMIS) emerged as an innovative approach that combines the principles of laparoscopic surgery with a transanal route [2]. By employing a single-port platform and standard laparoscopic instruments to establish a pneumorectum, TAMIS provides high-definition visualization and facilitates precise full-thickness excision of rectal lesions located up to ~10 cm from the anal verge [3].
This technique serves as a flexible and cost-effective alternative to transanal endoscopic microsurgery (TEM), offering similar oncologic and technical advantages without the need for specialized, high-cost equipment [4]. Multiple clinical series have demonstrated high rates of R0 resection and low postoperative morbidity with TAMIS in both benign lesions and selected T1 rectal cancers [5].
Case report
We present the case of a 48-year-old woman with a large mid-to-low rectal tubulovillous adenoma with focal high-grade dysplasia successfully excised using TAMIS. This report underscores the role of TAMIS as an organ-preserving, minimally invasive option for benign rectal tumors with advanced dysplasia.
A 48-year-old female with a history of thyroid cancer under active treatment presented with a several-month history of a foreign body sensation in the anal region, associated with occasional rectal bleeding. She denied weight loss or changes in bowel habits. Physical examination, including rigid rectoscopy, revealed a polypoid lesion located 3–4 cm from the anal verge. Laboratory parameters were within normal limits.
Pelvic magnetic resonance imaging (MRI) revealed a solid, stenosing lesion located 27 mm from the anal verge, extending from the 7 o’clock to 11 o’clock position, infiltrating the muscular layer but without mesorectal fascia invasion. The lesion measured 73 mm longitudinally and 51 mm in both anteroposterior and transverse diameters, located in the mid-to-low rectum, staged as T3N0M0 (Figs 1 and 2).
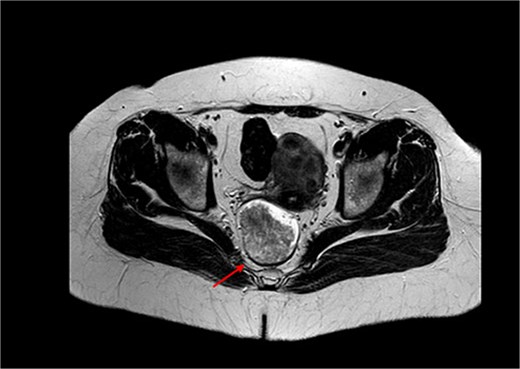
MRI of the pelvis in axial view demonstrating a solid, stenosing lesion located 27 mm from the anal verge. The lesion infiltrates the muscular layer between the 7 and 11 o’clock positions and causes changes in the intensity of the mesorectal fat without fascia involvement.
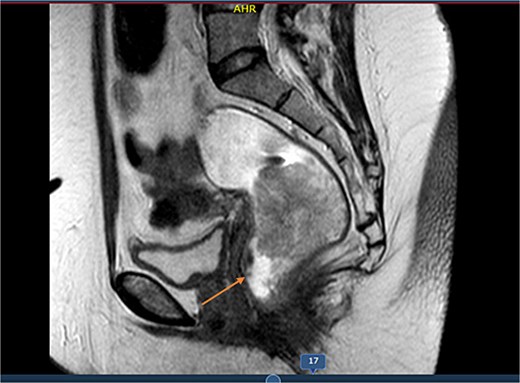
MRI sagittal view showing the longitudinal extent of the rectal lesion measuring ~73 mm in length, involving the mid-to-distal rectum, consistent with a T3N0M0 tumor staging.
Initial biopsy from rectoscopy showed a tubular adenoma with focal high-grade dysplasia and extensive low-grade dysplasia. Given the MRI findings, colonoscopy was prioritized, confirming a polypoid lesion 4 cm in diameter at 4 cm from the anal verge. Targeted biopsy revealed a tubular adenoma with high-grade dysplasia.
The patient underwent TAMIS under general anesthesia. Intraoperative findings included a friable, irregular tumor measuring ~5 cm in diameter. The base of the lesion was marked with a suture before excision (Figs 3 and 4). The specimen was removed en bloc.
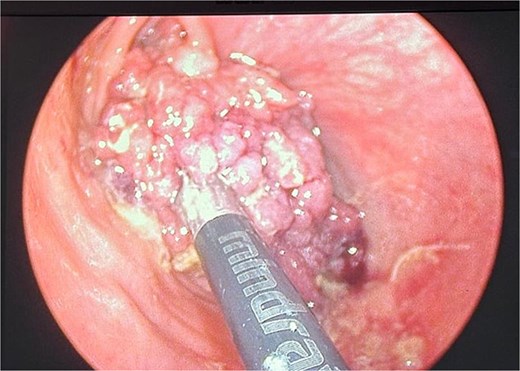
Intraoperative image during transanal minimally invasive surgery (TAMIS) showing the polypoid tumor with friable and irregular borders measuring ~5 cm. The base of the lesion is marked with a suture to guide excision.
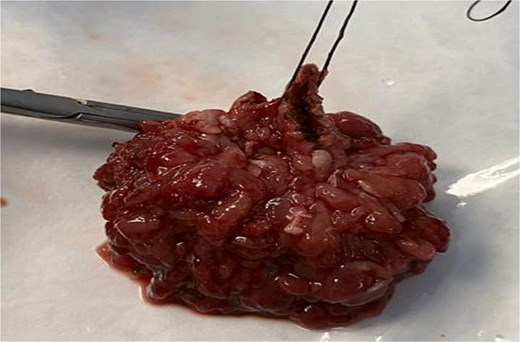
Resected specimen after TAMIS demonstrating the excised tubulovillous adenoma with clear margins, sent for histopathological evaluation.
Final pathology reported
Tubulovillous adenoma with focal high-grade dysplasia and low-grade dysplasia.
Negative resection margins
The procedure was completed without complications. Estimated blood loss was minimal. The patient was discharged the following day. At 72 h postoperatively, follow-up examination revealed a well-healed surgical site with no signs of infection or bleeding. At subsequent follow-ups, the patient remained asymptomatic, with no palpable masses on digital rectal examination.
Discussion
The management of benign rectal adenomas—especially those presenting with high-grade dysplasia—has evolved to favor organ-preserving techniques. Traditional TAE remains widely practiced, but its limitations include poor visualization, higher rates of positive margins, and elevated recurrence risk especially with lesions in the mid to upper rectum [1]. Advances in transanal surgery have introduced more effective alternatives.
TEM and TAMIS have consistently demonstrated superior outcomes compared to TAE. A network meta-analysis found that both TEM and TAMIS outperform TAE in terms of oncologic safety, with fewer positive margins and lower recurrence, as well as reduced morbidity and shorter hospital stays [2]. Moreover, TAMIS achieves comparable results to TEM—including R0 resection rates and complication profiles—but with reduced setup complexity and cost [3].
Retrospective series of TAMIS for rectal adenomas report acceptable safety profiles, with overall morbidity around 12%–19% and low rates of conversion to radical surgery. Tumor fragmentation and positive margins—potentially more frequent with larger lesions—remain challenges, but clear resection margins are achievable in most cases [4]. Our patient’s case aligns well with these findings: we successfully resected a 5-cm tubulovillous adenoma with focal high-grade dysplasia via TAMIS, achieving clear margins and no complications, reinforcing TAMIS as both safe and effective.
Emerging technologies such as robotic-assisted TAMIS (R-TAMIS) show promising enhancements [5]. In a comparative series, R-TAMIS was faster and achieved a 0% positive margin rate, outperforming both conventional TAMIS and TEM in this regard [6]. Though still in early adoption, these results hint at future directions for minimally invasive local excisions [7, 8].
Overall, our case underscores TAMIS as a valuable option in the current surgical armamentarium for rectal neoplasms with high-grade dysplasia—allowing organ preservation, low morbidity, and excellent oncologic control [9]. Nonetheless, continued surveillance is essential, especially for larger lesions, to monitor for recurrence [10].
Conflict of interest statement
None declared.
Funding
None declared.
References
Šemanjski K, Lužaić K, Brkić J.
Perivoliotis K, Baloyiannis I, Sarakatsianou C, et al. .
Hong KD, Kang S, Urn JW, et al. .
Haugvik SP, Groven S, Bondi J, et al. .
Schwab ME, Hernandez S, Watanaskul S, et al. .
- magnetic resonance imaging
- surgical procedures, minimally invasive
- biopsy
- colonoscopy
- physical examination
- adenoma
- adenoma, villous
- follow-up
- foreign bodies
- laboratory techniques and procedures
- muscle rigidity
- rectal neoplasms
- surgical procedures, operative
- anus
- fascia
- histology
- sensory perception
- rectal bleeding
- thyroid cancer
- perianal region
- surgical margins
- tubular adenoma
- excision
- magnetic resonance imaging of pelvis
- dysplasia
- tubulovillous adenoma
- transanal minimally invasive surgery
- undertreatment



